QoL and Patient-Reported Outcome and Supportive Care
Poster Session 3
P-478: Humanistic, Clinical, and Economic Burden in Patients with Relapsed or Refractory Multiple Myeloma on Second Line or Higher Therapy: A Systematic Literature Review
Friday, September 29, 2023
1:15 PM - 2:15 PM EEST

Kody Pierce, PharmD, MBA (he/him/his)
HEOR Scientist
AbbVie
Atlanta, Georgia, United States
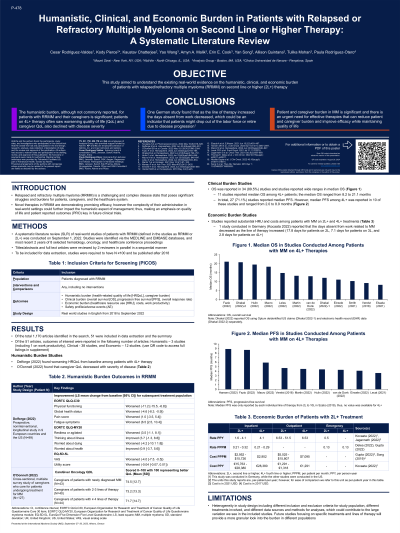
Introduction: Novel therapies in relapsed/refractory multiple myeloma (RRMM) are demonstrating promising efficacy, however the complexity of their administration in real-world settings could further impact the humanistic aspect of management; thus, making an emphasis on QOL and patient reported outcomes (PRO) key in future clinical trials. The objective of the study was to understand real-world evidence on the humanistic, clinical, and economic burden of RRMM.
Methods: A systematic literature review (SLR) was conducted to identify real-world studies of patients with RRMM from 2018 to September 1, 2022, with outcomes of interest. Studies were identified via the MEDLINE and EMBASE databases, and selected conference proceedings. All studies were required to have at least 100 patients. Titles/abstracts and full text articles were reviewed by 2 reviewers in parallel. Data were extracted from relevant articles and were descriptively summarized.
Results: Of the 1,170 studies identified, 51 were included in the review. The majority of the studies (n=38) reported clinical outcomes, 12 reported economic outcomes and 3 reported humanistic outcomes. Overall survival (OS) was included in most studies reporting clinical outcomes (34, 89.5%) with progression free survival (PFS) included in (27,71.1%) studies. The median OS of patients with 4L+ RRMM ranged from 8.2 to 21.1 months while the median PFS ranged from 2.0 to 8.9 months. The mean all-cause cost per patient per month ranged from $2,952-$15,726 for inpatient and $5,025-$15,807 for outpatient. Of studies identified on humanistic burden most focused on burden from the patient perspective including PROs and health related quality of life (HRQoL). However, some studies reported on humanistic burden from a macro or caregiver perspective including absenteeism and caregiver QoL. For patients with 4L+, thinking about illness, worried about health, and worried about dying PRO domains only worsened from baseline (N=87, LS mean change from BL was −7.5, −9.7, and −14.4 respectively). Another study reported on the diminished QoL for caregivers using the CareGiver Oncology QOL questionnaire (74.5 for newly diagnosed multiple myeloma [NDMM], 73.2 for 2-3L, and 71.7 for 4L+; scored 0-100 with 100 representing normal/better QoL).
Conclusions: The median OS for patients with 4L+ RRMM was less than 2 years, indicating that the 4L+ population continues to have a large unmet need for therapy options. Patient and caregiver burden in MM is significant and there is an urgent need for effective therapies that can reduce patient and caregiver burden and improve efficacy while maintaining quality of life.
Methods: A systematic literature review (SLR) was conducted to identify real-world studies of patients with RRMM from 2018 to September 1, 2022, with outcomes of interest. Studies were identified via the MEDLINE and EMBASE databases, and selected conference proceedings. All studies were required to have at least 100 patients. Titles/abstracts and full text articles were reviewed by 2 reviewers in parallel. Data were extracted from relevant articles and were descriptively summarized.
Results: Of the 1,170 studies identified, 51 were included in the review. The majority of the studies (n=38) reported clinical outcomes, 12 reported economic outcomes and 3 reported humanistic outcomes. Overall survival (OS) was included in most studies reporting clinical outcomes (34, 89.5%) with progression free survival (PFS) included in (27,71.1%) studies. The median OS of patients with 4L+ RRMM ranged from 8.2 to 21.1 months while the median PFS ranged from 2.0 to 8.9 months. The mean all-cause cost per patient per month ranged from $2,952-$15,726 for inpatient and $5,025-$15,807 for outpatient. Of studies identified on humanistic burden most focused on burden from the patient perspective including PROs and health related quality of life (HRQoL). However, some studies reported on humanistic burden from a macro or caregiver perspective including absenteeism and caregiver QoL. For patients with 4L+, thinking about illness, worried about health, and worried about dying PRO domains only worsened from baseline (N=87, LS mean change from BL was −7.5, −9.7, and −14.4 respectively). Another study reported on the diminished QoL for caregivers using the CareGiver Oncology QOL questionnaire (74.5 for newly diagnosed multiple myeloma [NDMM], 73.2 for 2-3L, and 71.7 for 4L+; scored 0-100 with 100 representing normal/better QoL).
Conclusions: The median OS for patients with 4L+ RRMM was less than 2 years, indicating that the 4L+ population continues to have a large unmet need for therapy options. Patient and caregiver burden in MM is significant and there is an urgent need for effective therapies that can reduce patient and caregiver burden and improve efficacy while maintaining quality of life.
