Cellular and T cell engager Immunotherapy
Poster Session 1
P-053: Idecabtagene vicleucel (ide-cel) retreatment response was characterized by poor activation, impaired cellular expansion, and limited cytolytic activity of chimeric antigen receptor (CAR) T cells
Wednesday, September 27, 2023
1:30 PM - 2:30 PM EEST
Fan Wu, PhD
Director, Clinical Pharmacology and Pharmacometrics
Bristol Myers Squibb, Princeton NJ, USA
Princeton, New Jersey, United States
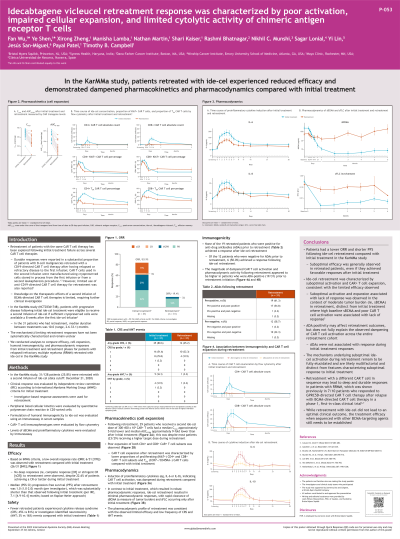
Introduction: Retreating patients with the same CAR T product has been explored across several CAR T products after progression during initial treatment. Suboptimal efficacy has generally been observed in retreated patients, even if they had achieved favorable responses after their first infusion. We conducted analyses to systematically compare overall response, cellular kinetics, humoral immunogenicity, and pharmacodynamic (PD) responses from initial and retreatment phases for patients retreated with ide-cel.
Methods: 31/128 patients (25.8%) were retreated with a second dose of ide-cel (12/21/2020 data cutoff) in the KarMMa study (NCT03361748). Peripheral blood cellular kinetics were evaluated by quantitative PCR in CD3-sorted cells. Formulation of humoral immunogenicity to ide-cel were evaluated using an immunoassay in serum samples. Immunophenotype of CAR+ T cells was evaluated by flow cytometry. Soluble BCMA (sBCMA) and proinflammatory cytokines were evaluated by immunoassay. Clinical response was evaluated using IMWG criteria.
Results: Low ORR (19.4%, 6/31) was observed with retreatment compared with initial treatment (83.9%, 26/31). Progression-free survival (PFS; median [95% CI]) after ide-cel retreatment was 1.0 (1.0–2.0) months, substantially shorter than PFS (7.1 [4.9–10.4] months) after initial ide-cel treatment. Fewer patients retreated with ide-cel experienced cytokine release syndrome (45.2% vs 80.6%) or investigator-identified neurotoxicity (3.2% vs 16%) than those on or after initial treatment. Induction of proinflammatory cytokines, indicating CAR T activation, was dampened during retreatment and minimal PD responses were observed. In 29 patients who received a second dose of ide-cel ranging from 300–450 x 10^6 CAR+ T cells, median Cmax following retreatment was 5.2-fold lower while median AUC0–28days was 8.6-fold lower than the initial infusion, despite most of the patients (23/29) receiving a higher target dose in the second infusion. CAR T cells expanding after retreatment were characterized by decreased proportions of CD4+ and CD8+ CAR+ subsets for proliferating (Ki67+) and TEM (CCR7−/CD45RA−) cells versus initial infusion. The magnitude of dampened CAR T activation and PD activity in retreatment trended higher in patients (19/31) who were anti-drug antibody (ADA) positive proximal to initiation of retreatment.
Conclusions: A lower ORR was observed in patients following ide-cel retreatment compared with initial treatment. Ide-cel retreatment was characterized by suboptimal activation and expansion, consistent with the limited efficacy observed. ADA may be implicated in retreatment but does not fully explain the observed CAR T activation dampening that was observed across the entire retreatment cohort. The mechanisms underlying suboptimal ide-cel activation during retreatment remain not fully elucidated and are likely multifactorial and distinct from features characterizing suboptimal response to initial infusion.
Methods: 31/128 patients (25.8%) were retreated with a second dose of ide-cel (12/21/2020 data cutoff) in the KarMMa study (NCT03361748). Peripheral blood cellular kinetics were evaluated by quantitative PCR in CD3-sorted cells. Formulation of humoral immunogenicity to ide-cel were evaluated using an immunoassay in serum samples. Immunophenotype of CAR+ T cells was evaluated by flow cytometry. Soluble BCMA (sBCMA) and proinflammatory cytokines were evaluated by immunoassay. Clinical response was evaluated using IMWG criteria.
Results: Low ORR (19.4%, 6/31) was observed with retreatment compared with initial treatment (83.9%, 26/31). Progression-free survival (PFS; median [95% CI]) after ide-cel retreatment was 1.0 (1.0–2.0) months, substantially shorter than PFS (7.1 [4.9–10.4] months) after initial ide-cel treatment. Fewer patients retreated with ide-cel experienced cytokine release syndrome (45.2% vs 80.6%) or investigator-identified neurotoxicity (3.2% vs 16%) than those on or after initial treatment. Induction of proinflammatory cytokines, indicating CAR T activation, was dampened during retreatment and minimal PD responses were observed. In 29 patients who received a second dose of ide-cel ranging from 300–450 x 10^6 CAR+ T cells, median Cmax following retreatment was 5.2-fold lower while median AUC0–28days was 8.6-fold lower than the initial infusion, despite most of the patients (23/29) receiving a higher target dose in the second infusion. CAR T cells expanding after retreatment were characterized by decreased proportions of CD4+ and CD8+ CAR+ subsets for proliferating (Ki67+) and TEM (CCR7−/CD45RA−) cells versus initial infusion. The magnitude of dampened CAR T activation and PD activity in retreatment trended higher in patients (19/31) who were anti-drug antibody (ADA) positive proximal to initiation of retreatment.
Conclusions: A lower ORR was observed in patients following ide-cel retreatment compared with initial treatment. Ide-cel retreatment was characterized by suboptimal activation and expansion, consistent with the limited efficacy observed. ADA may be implicated in retreatment but does not fully explain the observed CAR T activation dampening that was observed across the entire retreatment cohort. The mechanisms underlying suboptimal ide-cel activation during retreatment remain not fully elucidated and are likely multifactorial and distinct from features characterizing suboptimal response to initial infusion.
