Cellular and T cell engager Immunotherapy
Poster Session 1
P-008: Idecabtagene vicleucel (ide-cel) vs standard regimens in triple-class–exposed (TCE) relapsed and refractory multiple myeloma (RRMM): KarMMa-3 subgroup analysis in patients receiving bridging therapy
Wednesday, September 27, 2023
1:30 PM - 2:30 PM EEST

Hermann Einsele, MD, FRCP (he/him/his)
Clinic Director of Medicine
Universitätsklinikum Würzburg, Medizinische Klinik und Poliklinik II, Würzburg, Germany
Würzburg, Bayern, Germany
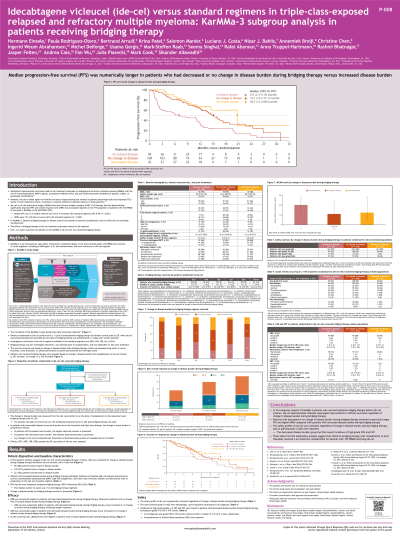
Introduction: Ide-cel, a BCMA-directed CAR T cell therapy (Tx), significantly improved median progression-free survival (mPFS; 13.3 vs 4.4 mo; HR 0.49; P< 0.001) and overall response rates (ORR; 71 vs 42%; P< 0.001) vs standard (std) regimens in patients (pts) with TCE RRMM in KarMMa-3 (NCT03651128). Optional bridging Tx (BTx) was allowed for disease control in pts randomized to ide-cel. Outcomes in pts in ide-cel arm who received BTx are reported.
Methods: Pts in KarMMa-3 randomized to ide-cel could receive ≤1 cycle of BTx, selected by investigator before randomization and dependent on last prior Tx. This post hoc analysis based disease burden (DB) on measurable disease pre-leukapheresis (LK; serum/urine M-protein, M-protein, or difference between involved/uninvolved free light chain). Pts who received BTx were grouped based on DB change from LK to ide-cel (≥25% increase; ≥25% decrease; no change). Efficacy (PFS, ORR, complete response rate [CRR], duration of response [DOR]) and safety of ide-cel were assessed.
Results: Of 254 pts randomized to ide-cel, 213 received BTx; 200 were evaluable for change in DB before ide-cel (DPd, n=45; DVd, n=20; IRd, n=25; Kd, n=26; EPd, n=59; other, n=25) (increase, n=59 [28%]; decrease, n=32 [15%]; no change, n=109 [51%]). Median number of cycles was 1 for all BTx regimens. A higher percentage of pts with increased disease had baseline high-risk MM characteristics (extramedullary plasmacytoma, increase, 41%; decrease, 16%; no change, 24%; high-risk cytogenetics, increase, 53%; decrease, 25%; no change, 38%; triple-class–refractory disease, increase, 90%; decrease, 63%; no change, 59%). mPFS (95% CI) was numerically longer in pts with decrease vs increase or no change (increase, 6.9 [2.4–11.8]; decrease, 20.7 [11.2–NR]; no change, 15.1 [12.4–17.3] mo). ORR (95% CI) was numerically higher in pts with decrease vs increase or no change (increase, 56% [43–69]; decrease, 97% [91–100]; no change, 80% [72–87]), with deeper (CRR: increase, 32%; decrease, 56%; no change, 39%), more durable (mDOR [95% CI]: increase, 9.3 [7.5–17.3]; decrease, 18.6 [8.6–NR]; no change, 12.9 [10.9–21.4] mo) responses. Any-grade (G; increase, 90%; decrease, 97%; no change, 96%) and G3/4 adverse event (AE; increase, 81%; decrease, 84%; no change, 95%) incidence was similar between groups. G5 AEs occurred in 15% (increase), 6% (decrease) and 13% (no change); serious AEs in 42%, 25%, and 44%, respectively. Any-G cytokine release syndrome occurred in 80% (increase), 94% (decrease), and 84% (no change); G3/4 in 7%, 3%, and 4%, respectively. Any-G investigator-identified neurotoxicity occurred in 24% (increase), 3% (decrease), and 13% (no change); G3/4 in 3%, 0%, and 4%, respectively.
Conclusions: Ide-cel resulted in longer mPFS and greater response in pts with TCE RRMM who had decrease/no change versus increase in DB with BTx. Regardless of change in DB, ide-cel safety profile was consistent. Effective BTx is an important consideration for ide-cel Tx in TCE RRMM.
Methods: Pts in KarMMa-3 randomized to ide-cel could receive ≤1 cycle of BTx, selected by investigator before randomization and dependent on last prior Tx. This post hoc analysis based disease burden (DB) on measurable disease pre-leukapheresis (LK; serum/urine M-protein, M-protein, or difference between involved/uninvolved free light chain). Pts who received BTx were grouped based on DB change from LK to ide-cel (≥25% increase; ≥25% decrease; no change). Efficacy (PFS, ORR, complete response rate [CRR], duration of response [DOR]) and safety of ide-cel were assessed.
Results: Of 254 pts randomized to ide-cel, 213 received BTx; 200 were evaluable for change in DB before ide-cel (DPd, n=45; DVd, n=20; IRd, n=25; Kd, n=26; EPd, n=59; other, n=25) (increase, n=59 [28%]; decrease, n=32 [15%]; no change, n=109 [51%]). Median number of cycles was 1 for all BTx regimens. A higher percentage of pts with increased disease had baseline high-risk MM characteristics (extramedullary plasmacytoma, increase, 41%; decrease, 16%; no change, 24%; high-risk cytogenetics, increase, 53%; decrease, 25%; no change, 38%; triple-class–refractory disease, increase, 90%; decrease, 63%; no change, 59%). mPFS (95% CI) was numerically longer in pts with decrease vs increase or no change (increase, 6.9 [2.4–11.8]; decrease, 20.7 [11.2–NR]; no change, 15.1 [12.4–17.3] mo). ORR (95% CI) was numerically higher in pts with decrease vs increase or no change (increase, 56% [43–69]; decrease, 97% [91–100]; no change, 80% [72–87]), with deeper (CRR: increase, 32%; decrease, 56%; no change, 39%), more durable (mDOR [95% CI]: increase, 9.3 [7.5–17.3]; decrease, 18.6 [8.6–NR]; no change, 12.9 [10.9–21.4] mo) responses. Any-grade (G; increase, 90%; decrease, 97%; no change, 96%) and G3/4 adverse event (AE; increase, 81%; decrease, 84%; no change, 95%) incidence was similar between groups. G5 AEs occurred in 15% (increase), 6% (decrease) and 13% (no change); serious AEs in 42%, 25%, and 44%, respectively. Any-G cytokine release syndrome occurred in 80% (increase), 94% (decrease), and 84% (no change); G3/4 in 7%, 3%, and 4%, respectively. Any-G investigator-identified neurotoxicity occurred in 24% (increase), 3% (decrease), and 13% (no change); G3/4 in 3%, 0%, and 4%, respectively.
Conclusions: Ide-cel resulted in longer mPFS and greater response in pts with TCE RRMM who had decrease/no change versus increase in DB with BTx. Regardless of change in DB, ide-cel safety profile was consistent. Effective BTx is an important consideration for ide-cel Tx in TCE RRMM.
