Myeloma Microenvironment and immune profiling
Poster Session 3
P-413: Inflammatory markers characterize neutrophils and C1q+ TAMs in the day 100 bone marrow aspirate post ASCT of patients with early progression
Friday, September 29, 2023
1:15 PM - 2:15 PM EEST

Caleb Stein, PhD
Research Associate
Mayo Clinic in Arizona
Scottsdale, Arizona, United States
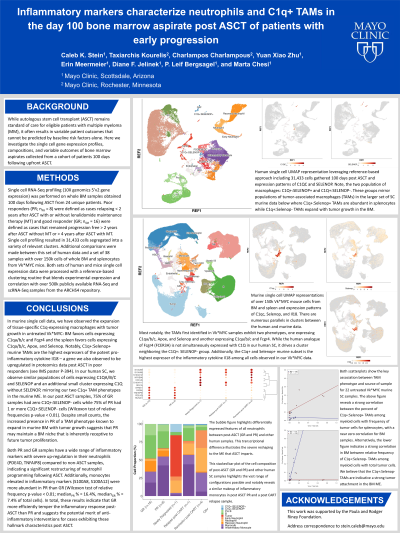
Introduction: Autologous stem cell transplant (ASCT) remains standard of care for eligible patients with multiple myeloma (MM), but it is associated with variable outcomes that cannot be predicted by baseline risk factors. Here we investigate the composition and expression features of bone marrow aspirates collected from a cohort of patients treated with upfront ASCT and sufficiently long follow up at single cell resolution.
Methods: To date, single cell RNA-Seq profiling (10X Genomics 5’v2 expression) has been performed on whole BM samples obtained 100 days following ASCT from 28 unique patients. Poor responders (PR; n=12) were defined as relapsing < 2yr after ASCT with or without lenalidomide maintenance treatment (MT) and good responders (GR) were defined as those who remained progression free for >2yr if not put on MT and >4yr if placed on MT (n=16). We compared these results with those obtained from whole BM or spleen samples collected from 67 Vk*MYC mice. Both sets of human and mice single cell data were processed with an additional reference-based clustering routine leveraging correlation with large, publicly available accession data from the ARCHS4 repository.
Results: We have observed the expansion of tissue-specific C1q+ macrophages along with MM growth in untreated Vk*MYC BM (expressing C1qa/b/c and Fcgr4) and spleen (expressing C1qa/b/c, Apoe, and Selenop) suggesting that these C1q+ cells represent a tumor-associated macrophage (TAM) phenotype specific to MM. Similarly, in our post-ASCT human samples, we detected a small group of cells that overexpress C1QA/B/C, APOE, and SELENOP that are more highly represented in the PR. Globally, C1q+ TAMs in our Vk*MYC set are the highest expressers of Il18 suggesting a crucial pro-inflammatory function of these distinct cells.
Neutrophils are highly involved in inflammatory response and demonstrate a gradient of maturation in Vk*MYC samples ranging from immature (expressing Camp and Ngp) to mature (expressing Il1b). Notably, some of the samples from GR were highly enriched for neutrophils that overexpressed markers of inhibition (PADI4, IRAK3, ANXA1) while those in the PR were up-regulated in pro-inflammatory markers such as FTH1. This result suggests that GR temper and control an inflammatory response directly post-ASCT while PR do not.
Conclusions: This research suggests the involvement of an inflammatory microenvironment in disease progression post ASCT. In clinical practice, observing key modulations in the myeloid compartment following ASCT could serve as an early detection method for identifying patients likely to progress who could be candidates for clinical trials of anti-inflammatory therapy to delay MM progression.
Methods: To date, single cell RNA-Seq profiling (10X Genomics 5’v2 expression) has been performed on whole BM samples obtained 100 days following ASCT from 28 unique patients. Poor responders (PR; n=12) were defined as relapsing < 2yr after ASCT with or without lenalidomide maintenance treatment (MT) and good responders (GR) were defined as those who remained progression free for >2yr if not put on MT and >4yr if placed on MT (n=16). We compared these results with those obtained from whole BM or spleen samples collected from 67 Vk*MYC mice. Both sets of human and mice single cell data were processed with an additional reference-based clustering routine leveraging correlation with large, publicly available accession data from the ARCHS4 repository.
Results: We have observed the expansion of tissue-specific C1q+ macrophages along with MM growth in untreated Vk*MYC BM (expressing C1qa/b/c and Fcgr4) and spleen (expressing C1qa/b/c, Apoe, and Selenop) suggesting that these C1q+ cells represent a tumor-associated macrophage (TAM) phenotype specific to MM. Similarly, in our post-ASCT human samples, we detected a small group of cells that overexpress C1QA/B/C, APOE, and SELENOP that are more highly represented in the PR. Globally, C1q+ TAMs in our Vk*MYC set are the highest expressers of Il18 suggesting a crucial pro-inflammatory function of these distinct cells.
Neutrophils are highly involved in inflammatory response and demonstrate a gradient of maturation in Vk*MYC samples ranging from immature (expressing Camp and Ngp) to mature (expressing Il1b). Notably, some of the samples from GR were highly enriched for neutrophils that overexpressed markers of inhibition (PADI4, IRAK3, ANXA1) while those in the PR were up-regulated in pro-inflammatory markers such as FTH1. This result suggests that GR temper and control an inflammatory response directly post-ASCT while PR do not.
Conclusions: This research suggests the involvement of an inflammatory microenvironment in disease progression post ASCT. In clinical practice, observing key modulations in the myeloid compartment following ASCT could serve as an early detection method for identifying patients likely to progress who could be candidates for clinical trials of anti-inflammatory therapy to delay MM progression.
