Other plasma cell disorders
Poster Session 3
P-443: Localised Light Chain (AL) Amyloidosis: Presentation, Treatment and Outcomes; an Observational Study.
Friday, September 29, 2023
1:15 PM - 2:15 PM EEST

Nirija Ranjit Anderson, MBBS
Clinical Haematology Fellow
Princess Alexandra Hospital, Queensland Health
Brisbane, Queensland, Australia
Introduction: Localised immunoglobulin light chain associated amyloid deposition is a rare disease. Tissue biopsy does not discriminate between localised and systemic forms of amyloidosis, thus clinical assessment of pattern of presentation, organ involvement and the presence or absence of a monoclonal component is required to discern between the two. Treatment recommendations are vastly different dependent on this diagnosis.
We report the clinical characteristics, treatment modalities and outcomes in patients with localised AL amyloidosis reviewed at a quaternary amyloidosis referral centre.
Methods: Database and medical records for all patients referred between January 2010 to May 2023 with a confirmed diagnosis of localised AL amyloidosis were reviewed. Demographic data, sites of organ involvement, treatment received, and recurrence or progression were assessed for each patient. Overall survival was estimated by the Kaplan-Meier method.
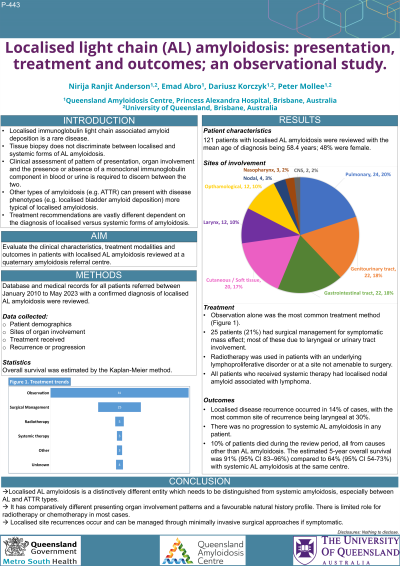
Results: 121 patients with localised AL amyloidosis were reviewed with the mean age of diagnosis being 58.4 years; 48% were female. The most common sites of presentation were pulmonary 20%, genitourinary and gastrointestinal tract with 18% each, followed by cutaneous/soft tissue 17%. Other commonly involved sites include the larynx and eye 10% each. Rarer sites were nodal 3%, central nervous system 2%, and nasopharynx 2%.
67% were treated with observation alone following their original biopsy. 21% had surgical management for symptomatic mass effect; the greatest proportion of these consisting of laryngeal or urinary tract involvement, with 28% and 24% respectively. 4% underwent radiotherapy for either an underlying lymphoproliferative disorder or for a site not amenable to surgery. 3% received systemic therapy (chemotherapy/immunotherapy), all were for localised nodal amyloid associated with lymphoma. 3% received other treatment options, such as autologous stem cell transplantation (for localised amyloid deposition associated with a plasmacytoma), topical therapy, or antiviral eradication therapy. The remaining 4% had incomplete records to enable assessment of treatment.
Localised disease recurrence occurred in 14% of cases, with the most common site of recurrence being laryngeal at 30%. There was no progression to systemic AL amyloidosis in any patient. 10% of patients died during the review period, all from causes other than AL amyloidosis. The estimated 5-year overall survival was 91% (95% CI 83–96%) compared to 64% (95% CI 54-73%) for systemic AL amyloidosis.
Conclusions: Localised AL amyloidosis is a distinctively different entity which needs to be distinguished from systemic amyloidosis, especially between AL and ATTR types. It has comparatively different presenting organ involvement patterns and a favourable natural history profile without active intervention in most cases. Localised site recurrences occur and can be managed through minimally invasive surgical approaches if symptomatic.
We report the clinical characteristics, treatment modalities and outcomes in patients with localised AL amyloidosis reviewed at a quaternary amyloidosis referral centre.
Methods: Database and medical records for all patients referred between January 2010 to May 2023 with a confirmed diagnosis of localised AL amyloidosis were reviewed. Demographic data, sites of organ involvement, treatment received, and recurrence or progression were assessed for each patient. Overall survival was estimated by the Kaplan-Meier method.
Results: 121 patients with localised AL amyloidosis were reviewed with the mean age of diagnosis being 58.4 years; 48% were female. The most common sites of presentation were pulmonary 20%, genitourinary and gastrointestinal tract with 18% each, followed by cutaneous/soft tissue 17%. Other commonly involved sites include the larynx and eye 10% each. Rarer sites were nodal 3%, central nervous system 2%, and nasopharynx 2%.
67% were treated with observation alone following their original biopsy. 21% had surgical management for symptomatic mass effect; the greatest proportion of these consisting of laryngeal or urinary tract involvement, with 28% and 24% respectively. 4% underwent radiotherapy for either an underlying lymphoproliferative disorder or for a site not amenable to surgery. 3% received systemic therapy (chemotherapy/immunotherapy), all were for localised nodal amyloid associated with lymphoma. 3% received other treatment options, such as autologous stem cell transplantation (for localised amyloid deposition associated with a plasmacytoma), topical therapy, or antiviral eradication therapy. The remaining 4% had incomplete records to enable assessment of treatment.
Localised disease recurrence occurred in 14% of cases, with the most common site of recurrence being laryngeal at 30%. There was no progression to systemic AL amyloidosis in any patient. 10% of patients died during the review period, all from causes other than AL amyloidosis. The estimated 5-year overall survival was 91% (95% CI 83–96%) compared to 64% (95% CI 54-73%) for systemic AL amyloidosis.
Conclusions: Localised AL amyloidosis is a distinctively different entity which needs to be distinguished from systemic amyloidosis, especially between AL and ATTR types. It has comparatively different presenting organ involvement patterns and a favourable natural history profile without active intervention in most cases. Localised site recurrences occur and can be managed through minimally invasive surgical approaches if symptomatic.
