Nursing Symposium
Poster Session 1
NSP-04: Managing Infections, Hypogammaglobulinemia, and Neutropenia During Treatment With Teclistamab in Relapsed/Refractory Multiple Myeloma: Nurse-Led Experience From the MajesTEC-1 Study
Wednesday, September 27, 2023
1:30 PM - 2:30 PM EEST

Donna Catamero, ANP-BC, OCN, CCRC
Associate Director, Myeloma Translational Research
Mount Sinai Health System, New York, NY, USA, United States
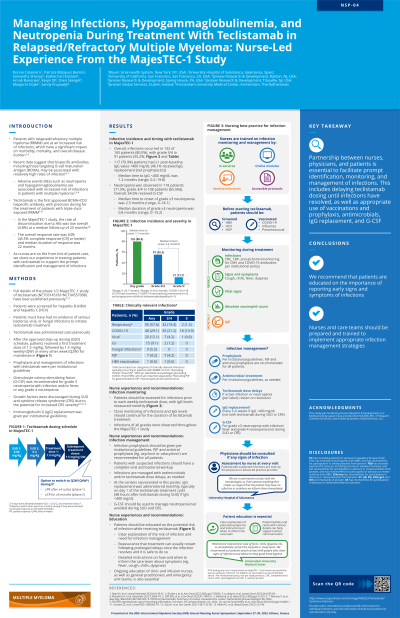
Introduction: Patients with relapsed/refractory multiple myeloma (RRMM) are at an increased risk of infection, which may compromise quality of life and treatment outcomes. Teclistamab is the only approved BCMA×CD3 bispecific antibody with a personalized, weight-based, and flexible dosing schedule for the treatment of triple-class exposed RRMM. In the MajesTEC-1 study, prophylaxis and management of infections with teclistamab were per institutional guidelines. We share our experience in managing patients treated with teclistamab to support nurses on the front line of patient care.
Methods: Patients in MajesTEC-1 were screened for hepatitis B and C, and must have had no evidence of serious bacterial, viral, or fungal infections to initiate treatment with teclistamab, which was administered subcutaneously at a dose of 1.5 mg/kg once weekly after the approved step-up dosing schedule. At our institutions, all patients treated with teclistamab were up to date with vaccinations (eg, COVID-19, influenza, and pneumococcal) and received acyclovir or valacyclovir prophylaxis; additional antimicrobials (eg, sulfamethoxazole/trimethoprim for Pneumocystis jirovecii pneumonia prophylaxis) were given per individual center guidelines. We regularly assessed all patients for infection prior to each weekly teclistamab dose and performed complete blood counts, cytomegalovirus testing, and COVID antibody testing as needed. Patients were also asked to self-report any signs or symptoms of infection (eg, fever, chills, cough) to the hospital team. Infections were managed with antimicrobials and teclistamab dose delays as appropriate. Immunoglobulin G (IgG) levels were monitored every 4 weeks at our centers with intravenous IgG (IVIG) given every 3–6 weeks if levels fell below 400 mg/dL. Treatment-emergent neutropenia was managed with granulocyte colony-stimulating factor (G-CSF), although this was avoided during periods of high risk for cytokine release syndrome, eg, teclistamab step-up dosing.
Results: In MajesTEC-1, infections occurred in 80.0% of patients, with grade 3/4 in 55.2% (most commonly COVID-19, respiratory infections, Pneumocystis jirovecii pneumonia, and viral infections) and deaths in 12.7%. Approximately 70% of patients had IgG < 400 mg/dL (overall, 46.1% received at least one dose of IVIG); 65.5% of patients had grade 3/4 neutropenia and 54.5% used G-CSF.
Conclusions: Teclistamab should not be given in case of any active infection; therefore, partnership between nurses, physicians, and patients is essential to facilitate prompt identification, monitoring, and management of infections, including appropriate use of antimicrobial prophylaxis, IVIG, and G-CSF. In particular, we recommend that patients are educated on the importance of reporting early signs and symptoms of infections, and that nurses and care teams are prepared and trained to implement appropriate infection management strategies.
Methods: Patients in MajesTEC-1 were screened for hepatitis B and C, and must have had no evidence of serious bacterial, viral, or fungal infections to initiate treatment with teclistamab, which was administered subcutaneously at a dose of 1.5 mg/kg once weekly after the approved step-up dosing schedule. At our institutions, all patients treated with teclistamab were up to date with vaccinations (eg, COVID-19, influenza, and pneumococcal) and received acyclovir or valacyclovir prophylaxis; additional antimicrobials (eg, sulfamethoxazole/trimethoprim for Pneumocystis jirovecii pneumonia prophylaxis) were given per individual center guidelines. We regularly assessed all patients for infection prior to each weekly teclistamab dose and performed complete blood counts, cytomegalovirus testing, and COVID antibody testing as needed. Patients were also asked to self-report any signs or symptoms of infection (eg, fever, chills, cough) to the hospital team. Infections were managed with antimicrobials and teclistamab dose delays as appropriate. Immunoglobulin G (IgG) levels were monitored every 4 weeks at our centers with intravenous IgG (IVIG) given every 3–6 weeks if levels fell below 400 mg/dL. Treatment-emergent neutropenia was managed with granulocyte colony-stimulating factor (G-CSF), although this was avoided during periods of high risk for cytokine release syndrome, eg, teclistamab step-up dosing.
Results: In MajesTEC-1, infections occurred in 80.0% of patients, with grade 3/4 in 55.2% (most commonly COVID-19, respiratory infections, Pneumocystis jirovecii pneumonia, and viral infections) and deaths in 12.7%. Approximately 70% of patients had IgG < 400 mg/dL (overall, 46.1% received at least one dose of IVIG); 65.5% of patients had grade 3/4 neutropenia and 54.5% used G-CSF.
Conclusions: Teclistamab should not be given in case of any active infection; therefore, partnership between nurses, physicians, and patients is essential to facilitate prompt identification, monitoring, and management of infections, including appropriate use of antimicrobial prophylaxis, IVIG, and G-CSF. In particular, we recommend that patients are educated on the importance of reporting early signs and symptoms of infections, and that nurses and care teams are prepared and trained to implement appropriate infection management strategies.
