Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-265: Mezigdomide (MEZI) monotherapy in relapsed/refractory multiple myeloma (RRMM): results from the CC-92480-MM-001 trial
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST

Scott R. Goldsmith, MD (he/him/his)
Hematologist
City Of Hope National Medical Center, Duarte, CA, USA, California, United States
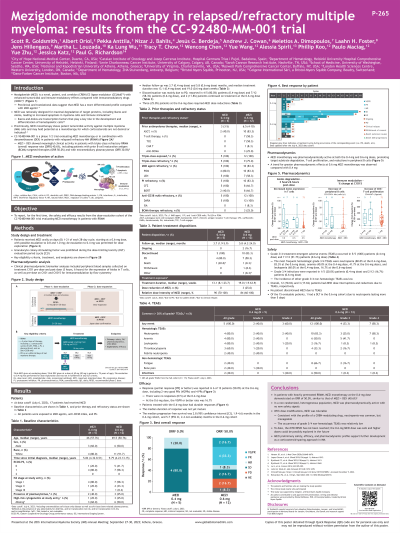
Introduction: MEZI is a novel oral cereblon E3 ligase modulator (CELMoD™) with enhanced antimyeloma effects compared with immunomodulatory drugs (IMiDs®). Preclinically, MEZI alone shows potent tumoricidal activity against MM cells and may hold potential as a monotherapy (e.g. where corticosteroids are not desired or indicated). Here we report results from the dose-escalation cohort of the CC-92480-MM-001 trial (NCT03374085) evaluating MEZI monotherapy in patients (pts) with RRMM.
Methods: Eligible pts had RRMM; ≥3 prior lines of therapy, including ≥2 consecutive cycles of lenalidomide, pomalidomide, a proteasome inhibitor (PI), a glucocorticoid, and an anti-CD38 monoclonal antibody; and disease progression on or within 60 days of last myeloma therapy. MEZI was started at 0.6mg, with possible escalation to 0.8 and 1.0mg, on days 1–21 of each 28-day cycle. De-escalation to 0.4mg was allowed if 0.6mg was not tolerated. Granulocyte-colony stimulating factor was prohibited during the dose-limiting toxicity (DLT) evaluation period (cycle 1). The primary objectives were safety, pharmacokinetics/pharmacodynamics (PD), and determination of the maximum tolerated dose (MTD) and recommended phase 2 dose (RP2D). Efficacy was an exploratory objective.
Results: As of March 22, 2023, 17 pts received MEZI (12 at 0.6mg, 5 at 0.4mg). Median age was 69 (50–76) years. Median number of prior therapies was 5 (3–10), including stem cell transplantation (70.6%); 14 (82.4%) pts were triple-class refractory. Median follow-up was 4.7 (0.4–12.0) months, median number of cycles received was 4 (1–12), and 4 (23.5%) pts were on treatment at data cutoff. Treatment discontinuation was mostly due to progressive disease (52.9%).
Grade (Gr) 3–4 treatment-emergent adverse events (TEAEs) occurred in 15 (88.2%) pts. The most frequent hematologic Gr 3–4 TEAEs were neutropenia (76.5%), anemia (41.2%), and leukopenia (29.4%). Gr 3–4 infections were reported in 2/17 pts; rates of other non-hematologic Gr 3–4 TEAEs were low. Twelve (70.6%) and 3 (17.6%) pts had MEZI dose interruptions and reductions due to TEAEs, respectively. No pts discontinued MEZI due to TEAEs. Of the 13 evaluable pts, 1 had a DLT (persistent Gr 4 neutropenia). To date, the MTD/RP2D has not been reached.
Overall response rate (ORR) at 0.6mg was 50.0% (6/12) with 1 complete response, 1 very good partial response, and 4 partial responses. Duration of response was immature. There were no responses (0/5) at 0.4mg.
MEZI monotherapy was pharmacodynamically active at both 0.4 and 0.6mg doses, promoting target substrate degradation, T-cell proliferation, and reductions in peripheral B cells.
Conclusions: In pts with heavily pretreated RRMM, MEZI monotherapy at the 0.6mg dose demonstrated a low incidence of severe non-hematologic toxicities with manageable cytopenias, and efficacy consistent with that of MEZI+DEX. Its preliminary safety, efficacy, and PD profile support further development as a corticosteroid-sparing approach in MM.
Methods: Eligible pts had RRMM; ≥3 prior lines of therapy, including ≥2 consecutive cycles of lenalidomide, pomalidomide, a proteasome inhibitor (PI), a glucocorticoid, and an anti-CD38 monoclonal antibody; and disease progression on or within 60 days of last myeloma therapy. MEZI was started at 0.6mg, with possible escalation to 0.8 and 1.0mg, on days 1–21 of each 28-day cycle. De-escalation to 0.4mg was allowed if 0.6mg was not tolerated. Granulocyte-colony stimulating factor was prohibited during the dose-limiting toxicity (DLT) evaluation period (cycle 1). The primary objectives were safety, pharmacokinetics/pharmacodynamics (PD), and determination of the maximum tolerated dose (MTD) and recommended phase 2 dose (RP2D). Efficacy was an exploratory objective.
Results: As of March 22, 2023, 17 pts received MEZI (12 at 0.6mg, 5 at 0.4mg). Median age was 69 (50–76) years. Median number of prior therapies was 5 (3–10), including stem cell transplantation (70.6%); 14 (82.4%) pts were triple-class refractory. Median follow-up was 4.7 (0.4–12.0) months, median number of cycles received was 4 (1–12), and 4 (23.5%) pts were on treatment at data cutoff. Treatment discontinuation was mostly due to progressive disease (52.9%).
Grade (Gr) 3–4 treatment-emergent adverse events (TEAEs) occurred in 15 (88.2%) pts. The most frequent hematologic Gr 3–4 TEAEs were neutropenia (76.5%), anemia (41.2%), and leukopenia (29.4%). Gr 3–4 infections were reported in 2/17 pts; rates of other non-hematologic Gr 3–4 TEAEs were low. Twelve (70.6%) and 3 (17.6%) pts had MEZI dose interruptions and reductions due to TEAEs, respectively. No pts discontinued MEZI due to TEAEs. Of the 13 evaluable pts, 1 had a DLT (persistent Gr 4 neutropenia). To date, the MTD/RP2D has not been reached.
Overall response rate (ORR) at 0.6mg was 50.0% (6/12) with 1 complete response, 1 very good partial response, and 4 partial responses. Duration of response was immature. There were no responses (0/5) at 0.4mg.
MEZI monotherapy was pharmacodynamically active at both 0.4 and 0.6mg doses, promoting target substrate degradation, T-cell proliferation, and reductions in peripheral B cells.
Conclusions: In pts with heavily pretreated RRMM, MEZI monotherapy at the 0.6mg dose demonstrated a low incidence of severe non-hematologic toxicities with manageable cytopenias, and efficacy consistent with that of MEZI+DEX. Its preliminary safety, efficacy, and PD profile support further development as a corticosteroid-sparing approach in MM.
