Myeloma Genomics and cell signaling
Poster Session 3
P-340: Minor clone of del(17p) provides a reservoir for relapse in multiple myeloma
Friday, September 29, 2023
1:15 PM - 2:15 PM EEST

Jian Cui
postgraduate
Institute of Hematology & Blood Diseases Hospital, Chinese Academy of Medical Science & Peking Union Medical College
Tianjin, Tianjin, China (People's Republic)
Introduction: As a secondary high-risk cytogenetic abnormality, The deletion of chromosome 17p [del(17p)], especially in high subclonal fraction, is associated with poor prognosis in multiple myeloma. Although del(17p) is detected in approximately 5-10% of newly diagnosed multiple myeloma (NDMM) patients, its prevalence increases to more than 10% in patients at relapse, mainly due to the emergence of new clones with acquired del(17p) during follow-up. However, the impact of del(17p) at relapse on survival at different clonal sizes remains unclear, despite the fact that patients who acquire del(17p) during follow-up have significantly shorter overall survival (OS) compared to controls. Furthermore, the patterns of clonal evolution of del(17p) between diagnosis and relapse and its prognostic value have not been fully understood.
Methods: The present study was based on the National Longitudinal Cohort of Hematological Diseases in China (NCT04645199). A total of 995 patients in the diagnosis dataset and 293 patients in the relapse dataset have been identified with the required cytogenetic data ( tested for chr1q gain, del(17p), del(13q), and IgH rearrangement). Among these patients, 197 had paired iFISH data at diagnosis and first relapse.
Results: We found a higher frequency of high-risk cytogenetic abnormalities (CAs) and more CAs in MM at relapse than those at diagnosis. Minor clone (present in 10%-50% of malignant PCs) of del(17p) at relapse (hazard ratio = 1.86) but not at diagnosis (hazard ratio = 1.39) was associated with a poor prognosis in MM. Our analysis of paired iFISH results revealed that 56 and 12 patients developed one or more than one new CAs at relapse, with the majority being secondary cytogenetic events, such as del(17p) and gain/amp(1q).
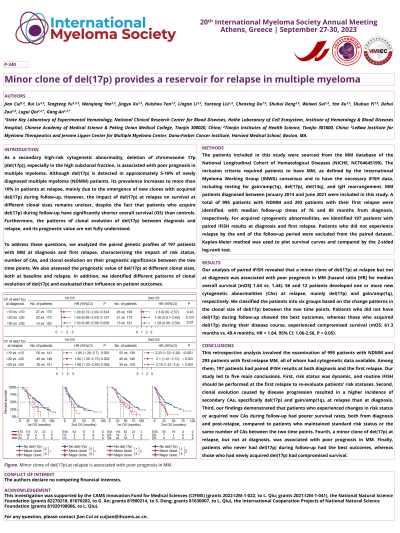
We then classified patients into six groups based on the change patterns in clonal size of del(17p) between the two time points. Patients in group A, who experienced the loss of del(17p) at relapse, as well as those in group B, who had a decreasing clonal size from the major to the minor clone at relapse, and those in group C, who did not have del(17p) at both time points, all had similarly superior outcomes (with a second OS of 50.3 months, 16.6 months, and 26.9 months, respectively). In contrast, patients in group D, who newly acquired del(17p) at relapse, had a relatively worse survival (with a second OS of 20.2 months). Of the remaining 16 patients, those with a stable clone of del(17p) between two time points (group E) and those with an obvious increase in clonal size of del(17p) (group F) both had the poorest outcomes (with a second OS of 12.5 months and 12.8 months, respectively).
Conclusions: In conclusion, our data confirmed the adverse impact of a minor clone of del(17p) at relapse and highlighted the importance of designing optimal therapeutic strategies to eliminate high-risk CAs.
Methods: The present study was based on the National Longitudinal Cohort of Hematological Diseases in China (NCT04645199). A total of 995 patients in the diagnosis dataset and 293 patients in the relapse dataset have been identified with the required cytogenetic data ( tested for chr1q gain, del(17p), del(13q), and IgH rearrangement). Among these patients, 197 had paired iFISH data at diagnosis and first relapse.
Results: We found a higher frequency of high-risk cytogenetic abnormalities (CAs) and more CAs in MM at relapse than those at diagnosis. Minor clone (present in 10%-50% of malignant PCs) of del(17p) at relapse (hazard ratio = 1.86) but not at diagnosis (hazard ratio = 1.39) was associated with a poor prognosis in MM. Our analysis of paired iFISH results revealed that 56 and 12 patients developed one or more than one new CAs at relapse, with the majority being secondary cytogenetic events, such as del(17p) and gain/amp(1q).
We then classified patients into six groups based on the change patterns in clonal size of del(17p) between the two time points. Patients in group A, who experienced the loss of del(17p) at relapse, as well as those in group B, who had a decreasing clonal size from the major to the minor clone at relapse, and those in group C, who did not have del(17p) at both time points, all had similarly superior outcomes (with a second OS of 50.3 months, 16.6 months, and 26.9 months, respectively). In contrast, patients in group D, who newly acquired del(17p) at relapse, had a relatively worse survival (with a second OS of 20.2 months). Of the remaining 16 patients, those with a stable clone of del(17p) between two time points (group E) and those with an obvious increase in clonal size of del(17p) (group F) both had the poorest outcomes (with a second OS of 12.5 months and 12.8 months, respectively).
Conclusions: In conclusion, our data confirmed the adverse impact of a minor clone of del(17p) at relapse and highlighted the importance of designing optimal therapeutic strategies to eliminate high-risk CAs.
