MRD Assessment and role in Myeloma
Poster Session 1
P-078: MRDeep Study: Measurable Residual Disease rates in patients with Multiple Myeloma who achieved complete response in 2nd or 3rd lines of treatment.
Wednesday, September 27, 2023
1:30 PM - 2:30 PM EEST

Manuel Neves (he/him/his)
Clinical Hematologist
Fundação Champalimaud: Hemato-Oncology Unit, Lisboa, Portugal
Introduction: Measurable Residual Disease (MRD) is rapidly becoming one of the most relevant prognostics indicators for patients with multiple myeloma (MM). The main objective of this cross-sectional, multicenter, non-interventional study was to evaluate the bone marrow MRD status in MM patients in Portugal who had achieved CR and were on their second or third lines of therapy.
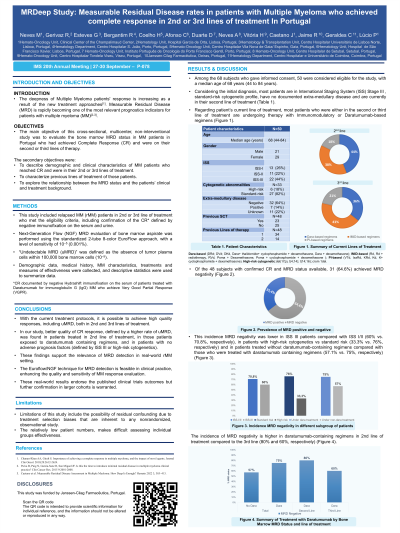
Methods: This study includes relapsed MM (rMM) patients in 2nd or 3rd line of treatment who met the eligibility criteria, including confirmation of the CR defined by negative immunofixation on the serum and urine. Next-Generation Flow (NGF) MRD evaluation of bone marrow aspirate was performed using the standardized 2-tube 8-color EuroFlow approach, with a level of sensitivity of 10^-5 (0.001%). “Undetectable MRD (uMRD)” was defined as the absence of tumor plasma cells within 100,000 bone marrow cells (10^-5). Demographic data, medical history, MM characteristics, treatments and measures of effectiveness were collected, and descriptive statistics were used to summarize data.
Results: Among the 68 subjects who gave informed consent, 48 were considered eligible for the study, with a median age of 68 (44 to 84 years). Twenty-two (44%) patients had ISS stage III disease, 6 out of 33 patients with available data had a high-risk cytogenetic profile (18.2%) and 7 out of 48 have documented extra-medullary disease (EMD) (14.5%). Of the 48 subjects with confirmed CR, 31 (64.6%) achieved MRD negativity. This incidence was lower in ISS III patients compared with ISS I/II (60% vs. 70.8%, respectively), in patients with high-risk cytogenetics vs. standard risk (33.3% vs. 76%, respectively) and in patients treated without daratumumab-containing regimens compared with those who were treated with daratumumab containing regimens (MRD undetectable in 57.1% and 75%, respectively). The incidence of MRD negativity is higher in daratumumab-containing regimens in 2nd line of treatment compared to the 3rd line (80% and 60%, respectively).
Conclusions: With the current treatment protocols it is possible to achieve high quality responses, including uMRD, both in 2nd and 3rd lines of treatment. In our study, better quality of CR response, defined by a higher rate of uMRD, was found in patients treated in 2nd line of treatment, in those patients exposed to daratumumab containing regimens, and in patients with no adverse prognosis factors (defined by ISS III or high-risk cytogenetics). These findings support the relevance of MRD detection in real-world rMM setting. The Euroflow/NGF technique for MRD detection is feasible in clinical practice, enhancing the quality and sensitivity of MM response evaluation. These real-world results endorse the published clinical trials outcomes but further confirmation in larger cohorts is warranted.
Methods: This study includes relapsed MM (rMM) patients in 2nd or 3rd line of treatment who met the eligibility criteria, including confirmation of the CR defined by negative immunofixation on the serum and urine. Next-Generation Flow (NGF) MRD evaluation of bone marrow aspirate was performed using the standardized 2-tube 8-color EuroFlow approach, with a level of sensitivity of 10^-5 (0.001%). “Undetectable MRD (uMRD)” was defined as the absence of tumor plasma cells within 100,000 bone marrow cells (10^-5). Demographic data, medical history, MM characteristics, treatments and measures of effectiveness were collected, and descriptive statistics were used to summarize data.
Results: Among the 68 subjects who gave informed consent, 48 were considered eligible for the study, with a median age of 68 (44 to 84 years). Twenty-two (44%) patients had ISS stage III disease, 6 out of 33 patients with available data had a high-risk cytogenetic profile (18.2%) and 7 out of 48 have documented extra-medullary disease (EMD) (14.5%). Of the 48 subjects with confirmed CR, 31 (64.6%) achieved MRD negativity. This incidence was lower in ISS III patients compared with ISS I/II (60% vs. 70.8%, respectively), in patients with high-risk cytogenetics vs. standard risk (33.3% vs. 76%, respectively) and in patients treated without daratumumab-containing regimens compared with those who were treated with daratumumab containing regimens (MRD undetectable in 57.1% and 75%, respectively). The incidence of MRD negativity is higher in daratumumab-containing regimens in 2nd line of treatment compared to the 3rd line (80% and 60%, respectively).
Conclusions: With the current treatment protocols it is possible to achieve high quality responses, including uMRD, both in 2nd and 3rd lines of treatment. In our study, better quality of CR response, defined by a higher rate of uMRD, was found in patients treated in 2nd line of treatment, in those patients exposed to daratumumab containing regimens, and in patients with no adverse prognosis factors (defined by ISS III or high-risk cytogenetics). These findings support the relevance of MRD detection in real-world rMM setting. The Euroflow/NGF technique for MRD detection is feasible in clinical practice, enhancing the quality and sensitivity of MM response evaluation. These real-world results endorse the published clinical trials outcomes but further confirmation in larger cohorts is warranted.
