QoL and Patient-Reported Outcome and Supportive Care
Poster Session 3
P-469: Observational study of COVID-19 prophylactic antibody (Tixagevimab/Cilgavimab) administration for multiple myeloma patients
Friday, September 29, 2023
1:15 PM - 2:15 PM EEST

Yoo Jin Lee, MD
Assistant professor
Department of Internal Medicine, Ulsan University Hospital, University of Ulsan College of Medicine
Ulsan, Republic of Korea
Introduction: The risk of COVID-19-associated morbidity and mortality among Multiple myeloma (MM) patients remains high during the post-pandemic COVID-19 period. In particular, autologous stem cell transplantation (ASCT) recipients or heavily treated patients may have a diminished response to COVID-19 vaccines. Therefore, we evaluated the efficacy and toxicity of neutralizing antibodies composed of tixagevimab and cilgavimab in the real world.
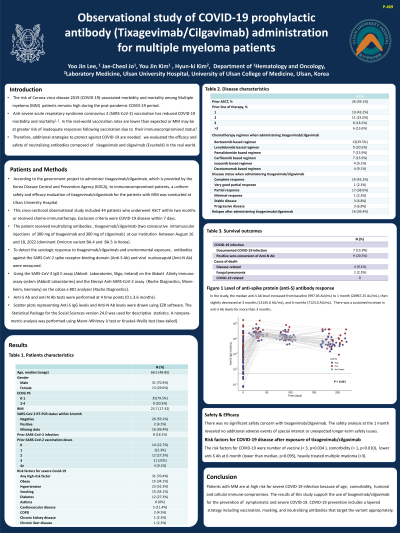
Methods: This cross-sectional observational study included 44 patients who received neutralizing antibodies to prevent COVID-19 at our institution between August 16 and 18, 2022 (dominant Omicron variant BA.4, BA.5 in Korea). The patient received tixagevimab/cilgavimab (two consecutive intramuscular injections of 300 mg of tixagevimab and 300 mg of cilgavimab). To detect the serologic response to tixagevimab/cilgavimab and environmental exposure, antibodies against the SARS CoV-2 spike receptor-binding domain (Anti-S Ab) and viral nucleocapsid (Anti-N Ab) were measured. Anti-S ab and anti-N ab tests were performed at 4 time points (0.1.3.6 months).
Results: A total of 44 MM patients underwent ASCT within two months or received chemo-immunotherapy (median second-line therapy). The median age was 68.5 years (48~ 85 years), and the male was 53.4%. Eight patients (18.2%) had previously confirmed COVID-19 infection. Twenty eight patients (63.6%) had previously received COVID-19 vaccination. In the study, the median anti-S Ab level increased from baseline (997.05 AU/mL) to 1 month (20967.25 AU/mL), then decreased at 3 months (13145.0 AU/mL), and 6 months (7123.0 AU/mL). Fourteen patients (31.8%) had positive anti-N Ab at baseline. There was no significant safety concern with tixagevimab/cilgavimab. Seven patients (15.9%) were infected with COVID-19 after exposure of tixagevimab/cilgavimab. The risk factors for COVID-19 were number of vaccine ( < 3, p=0.034 ), comorbidity (> 1, p=0.010), lower anti-S Ab at 6 month (lower than median, p=0.095), heavily treated multiple myeloma (>3). There was no COVID-19 related mortality.
Conclusions: Patients with MM are at high risk for severe COVID-19 infection because of age, comorbidity, humoral and cellular immune-compromises. The results of this study support the use of tixagevimab/cilgavimab for the prevention of symptomatic and severe COVID-19. COVID-19 prevention includes a layered strategy including vaccination, masking, and neutralizing antibodies that target the variant appropriately.
Methods: This cross-sectional observational study included 44 patients who received neutralizing antibodies to prevent COVID-19 at our institution between August 16 and 18, 2022 (dominant Omicron variant BA.4, BA.5 in Korea). The patient received tixagevimab/cilgavimab (two consecutive intramuscular injections of 300 mg of tixagevimab and 300 mg of cilgavimab). To detect the serologic response to tixagevimab/cilgavimab and environmental exposure, antibodies against the SARS CoV-2 spike receptor-binding domain (Anti-S Ab) and viral nucleocapsid (Anti-N Ab) were measured. Anti-S ab and anti-N ab tests were performed at 4 time points (0.1.3.6 months).
Results: A total of 44 MM patients underwent ASCT within two months or received chemo-immunotherapy (median second-line therapy). The median age was 68.5 years (48~ 85 years), and the male was 53.4%. Eight patients (18.2%) had previously confirmed COVID-19 infection. Twenty eight patients (63.6%) had previously received COVID-19 vaccination. In the study, the median anti-S Ab level increased from baseline (997.05 AU/mL) to 1 month (20967.25 AU/mL), then decreased at 3 months (13145.0 AU/mL), and 6 months (7123.0 AU/mL). Fourteen patients (31.8%) had positive anti-N Ab at baseline. There was no significant safety concern with tixagevimab/cilgavimab. Seven patients (15.9%) were infected with COVID-19 after exposure of tixagevimab/cilgavimab. The risk factors for COVID-19 were number of vaccine ( < 3, p=0.034 ), comorbidity (> 1, p=0.010), lower anti-S Ab at 6 month (lower than median, p=0.095), heavily treated multiple myeloma (>3). There was no COVID-19 related mortality.
Conclusions: Patients with MM are at high risk for severe COVID-19 infection because of age, comorbidity, humoral and cellular immune-compromises. The results of this study support the use of tixagevimab/cilgavimab for the prevention of symptomatic and severe COVID-19. COVID-19 prevention includes a layered strategy including vaccination, masking, and neutralizing antibodies that target the variant appropriately.
