QoL and Patient-Reported Outcome and Supportive Care
Poster Session 3
P-480: Outcome of Pneumocystis jirovecii pneumonia in patients with multiple myeloma
Friday, September 29, 2023
1:15 PM - 2:15 PM EEST

Christine Riedhammer, MD (she/her/hers)
Physician
University Hospital Würzburg, United States
Introduction: Patients with multiple myeloma (MM) are at high risk for infections, including opportunistic infections such as Pneumocystis jirovecii pneumonia (PJP). We conducted a retrospective analysis of patients with MM developing PJP over a six-year period at the University Hospital of Würzburg.
Methods: Between January 2016 and December 2021, positive results for P. jirovecii in respiratory specimens were retrospectively retrieved through our microbiology database as a quality improvement project in cooperation between the in-house antimicrobial stewardship team (AMS) and the department of hematology. Cases were screened for patients with MM and diagnoses of probable and proven PJP were assessed according to EORTC invasive fungal disease definitions. Patient characteristics, diagnostic findings, disease course, outcome and use of PJP prophylaxis were analyzed in PJP patients.
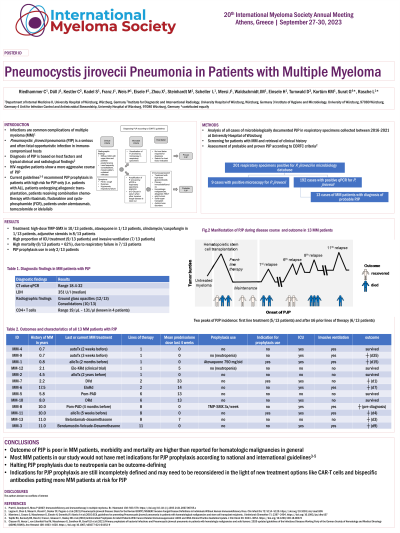
Results: From 2016 to 2021, 201 respiratory specimens were tested positive for P. jirovecii. Of these cases, 13 patients with a diagnosis of MM fulfilled the definition of probable PJP. We observed two peaks of PJP incidence, one in patients after autologous or allogeneic transplantation during first line treatment (n = 5), the other in heavily pretreated patients with six or more prior lines of therapy (n = 6). There was high morbidity with nine (69%) patients admitted to the ICU with seven of those (78%) requiring mechanical ventilation, and high mortality (62%, n = 8) within four weeks after PJP diagnosis or due to PJP-related complications, partly complicated by CMV or HSV reactivation (n = 3). Of note, only two of the 13 (15%) patients had received PJP prophylaxis. The main reason for halting prophylaxis with trimethoprim-sulfomethoxazole was grade IV neutropenia.
Conclusions: PJP can occur in every treatment phase of MM, but mainly affects patients after stem cell transplantation and heavily pretreated patients. Morbidity and mortality in MM patients are significant and even higher than reported for patients with hematologic malignancy in general. Indication for PJP prophylaxis is still incompletely defined, even in HIV-negative patients, but should be assessed individually in patients with risk factors, and halting PJP prophylaxis due to leukopenia needs to be reconsidered. According to current guidelines, prophylaxis use would have been clearly recommended in no more than three (23%) of the 13 patients.
Methods: Between January 2016 and December 2021, positive results for P. jirovecii in respiratory specimens were retrospectively retrieved through our microbiology database as a quality improvement project in cooperation between the in-house antimicrobial stewardship team (AMS) and the department of hematology. Cases were screened for patients with MM and diagnoses of probable and proven PJP were assessed according to EORTC invasive fungal disease definitions. Patient characteristics, diagnostic findings, disease course, outcome and use of PJP prophylaxis were analyzed in PJP patients.
Results: From 2016 to 2021, 201 respiratory specimens were tested positive for P. jirovecii. Of these cases, 13 patients with a diagnosis of MM fulfilled the definition of probable PJP. We observed two peaks of PJP incidence, one in patients after autologous or allogeneic transplantation during first line treatment (n = 5), the other in heavily pretreated patients with six or more prior lines of therapy (n = 6). There was high morbidity with nine (69%) patients admitted to the ICU with seven of those (78%) requiring mechanical ventilation, and high mortality (62%, n = 8) within four weeks after PJP diagnosis or due to PJP-related complications, partly complicated by CMV or HSV reactivation (n = 3). Of note, only two of the 13 (15%) patients had received PJP prophylaxis. The main reason for halting prophylaxis with trimethoprim-sulfomethoxazole was grade IV neutropenia.
Conclusions: PJP can occur in every treatment phase of MM, but mainly affects patients after stem cell transplantation and heavily pretreated patients. Morbidity and mortality in MM patients are significant and even higher than reported for patients with hematologic malignancy in general. Indication for PJP prophylaxis is still incompletely defined, even in HIV-negative patients, but should be assessed individually in patients with risk factors, and halting PJP prophylaxis due to leukopenia needs to be reconsidered. According to current guidelines, prophylaxis use would have been clearly recommended in no more than three (23%) of the 13 patients.
