MRD Assessment and role in Myeloma
Poster Session 1
P-086: Patient and Haematologist Perspectives of Minimal Residual Disease Testing in Myeloma
Wednesday, September 27, 2023
1:30 PM - 2:30 PM EEST

Silène ten Seldam, MSc (she/her/hers)
Research Assistant
Myeloma Patients Europe, United States
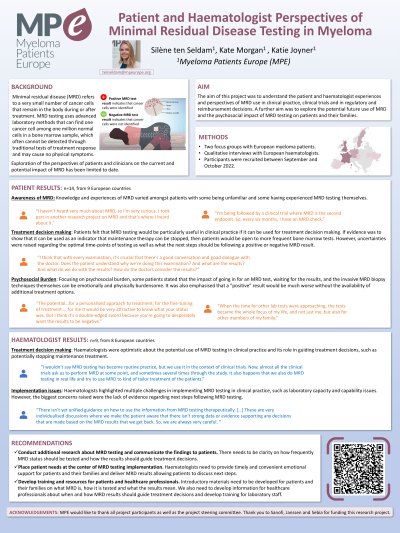
Introduction: Minimal residual disease (MRD) refers to a very small number of cancer cells that remain in the body during or after treatment. Despite growing interest of MRD in clinical practice and clinical trials, little is known regarding the perspectives and experiences of MRD testing from haematologists and myeloma patients. This project captured these perspectives on the current and potential future use of MRD in clinical practice and the psychosocial impact of MRD testing on patients and families.
Methods: Participants were recruited from across Europe through patient organisations, website and via email. Two focus groups with myeloma patients were held along with individual interviews with haematologists. Focus groups and interviews were online and conducted using semi-structured topic guides, informed by a review of existing literature. Discussions were recorded, transcribed, and thematically analysed.
Results: The focus group discussions with patients (n=14, from 9 countries) included 3 key themes; awareness of MRD, MRD-informed treatment decision making, and the potential psychosocial burden. Awareness of MRD testing varied amongst patients with some unfamiliar and some having experienced MRD testing themselves. Patients felt optimistic about MRD testing, particularly if it can be used for treatment decision making. Patients expressed willingness to consider more frequent bone marrow tests if MRD results could be used as an indicator for maintenance therapy to be stopped. However, they also highlighted the potential emotional and physical burden of attending hospital for the MRD tests, the invasive biopsies required, and the discomfort of waiting for the results. It was also emphasised that a positive MRD result, in the context of no available further treatments, would be particularly hard for patients.
The interviews with haematologists (n=9, from 8 countries) included themes on MRD-informed treatment decision making, and MRD implementation considerations. Haematologists were equally optimistic about the potential for MRD testing in clinical practice and its role in guiding treatment decisions such as maintenance treatment plans. However, they also highlighted multiple challenges in implementing MRD testing in clinical practice, such as laboratory capacity and capability issues, the cost and staff training.
Conclusions: This research highlighted that patients may be unaware of MRD testing, and there is a need for resources for patients and families to facilitate understanding about what it is and the implications of results. Implementation of MRD testing in future clinical practice would also require training and resources for healthcare professionals and laboratory staff to ensure accuracy and consistency across testing centres. The emotional and physical impact of MRD testing on patients will also need to be considered and healthcare providers need to be mindful of this in their communication and care of myeloma patients.
Methods: Participants were recruited from across Europe through patient organisations, website and via email. Two focus groups with myeloma patients were held along with individual interviews with haematologists. Focus groups and interviews were online and conducted using semi-structured topic guides, informed by a review of existing literature. Discussions were recorded, transcribed, and thematically analysed.
Results: The focus group discussions with patients (n=14, from 9 countries) included 3 key themes; awareness of MRD, MRD-informed treatment decision making, and the potential psychosocial burden. Awareness of MRD testing varied amongst patients with some unfamiliar and some having experienced MRD testing themselves. Patients felt optimistic about MRD testing, particularly if it can be used for treatment decision making. Patients expressed willingness to consider more frequent bone marrow tests if MRD results could be used as an indicator for maintenance therapy to be stopped. However, they also highlighted the potential emotional and physical burden of attending hospital for the MRD tests, the invasive biopsies required, and the discomfort of waiting for the results. It was also emphasised that a positive MRD result, in the context of no available further treatments, would be particularly hard for patients.
The interviews with haematologists (n=9, from 8 countries) included themes on MRD-informed treatment decision making, and MRD implementation considerations. Haematologists were equally optimistic about the potential for MRD testing in clinical practice and its role in guiding treatment decisions such as maintenance treatment plans. However, they also highlighted multiple challenges in implementing MRD testing in clinical practice, such as laboratory capacity and capability issues, the cost and staff training.
Conclusions: This research highlighted that patients may be unaware of MRD testing, and there is a need for resources for patients and families to facilitate understanding about what it is and the implications of results. Implementation of MRD testing in future clinical practice would also require training and resources for healthcare professionals and laboratory staff to ensure accuracy and consistency across testing centres. The emotional and physical impact of MRD testing on patients will also need to be considered and healthcare providers need to be mindful of this in their communication and care of myeloma patients.
