Cellular and T cell engager Immunotherapy
Poster Session 1
P-013: Patterns of Cytokine Release Syndrome with Teclistamab in Relapsed/Refractory Multiple Myeloma with or without Prior T-Cell Redirection Therapy.
Wednesday, September 27, 2023
1:30 PM - 2:30 PM EEST
- IH
Issam S. Hamadeh, PharmD (he/him/his)
Clinical pharmacy specialist
Memorial Sloan Kettering Cancer Center, New York City NY, USA
New York, New York, United States
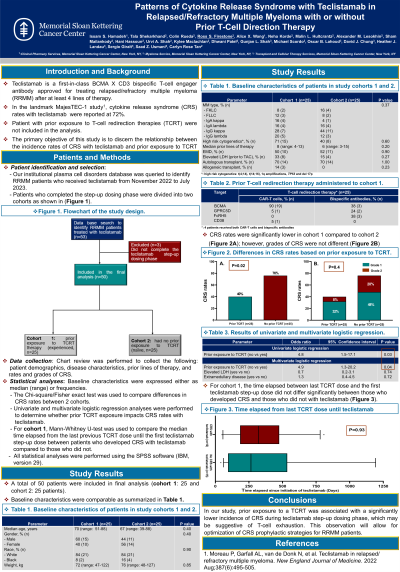
Introduction: Teclistamab (Tec) is a first-in-class BCMA X CD3 bispecific T-cell engager antibody approved for treating relapsed/refractory multiple myeloma (RRMM) after at least 4 lines of therapy (LOT). In the landmark MajesTEC-1 study, cytokine release syndrome (CRS) rate with Tec was 72% (Usmani S, et al. Lancet 2021, Moreau P, et al. N Engl J Med 2022), but patients who previously received T-cell redirection therapies were excluded (TCRT: CAR T-cells and/or other bispecific antibodies). Given this knowledge gap, we examined whether prior TCRT exposure impacts CRS rates with Tec in a real-world setting.
Methods: Our institutional plasma cell disorders database was queried to identify RRMM patients who received commercial Tec from November 2022 to May 2023. Patients who completed the step-up dosing phase (first step-up, second step-up and first full doses) were divided into two cohorts based on TCRT exposure before Tec (prior TCRT exposure: cohort 1 and no prior TCRT exposure: cohort 2). Data collection included patient demographics, disease characteristics, prior LOT, and rates/grades of CRS and ICANS. The Chi-square/Fisher exact test was used to compare differences in CRS rates between the two cohorts. Univariate and multivariate logistic regression analyses were performed to assess impact of prior TCRT exposure on CRS rates with Tec. Statistical analysis was performed using SPSS software (version 29).
Results: 41 patients (cohort 1: 21 and cohort 2: 20) were included in the final analysis. Baseline characteristics were comparable between the two cohorts except for previous LOT: 8 (range: 4-13) in cohort 1 and 6 (range: 3-15) in cohort 2 (p=0.02). High-risk cytogenetic abnormalities [t (4;14), t (14;16), t (14;20), TP53 mutations, del 17p and 1q amplification) were present in 71% (n=15) and 40% (n=8) of patients in cohorts 1 and 2, respectively (p=0.06). Extramedullary disease (EMD) was present in 57% (n=12) of patients in cohort 1 and 50% (n=10) in cohort 2. Elevated LDH (prior to teclistamab) was seen in 33% (n=7) of patients in cohort 1 and 15% (n=3) in cohort 2 (p=0.27). CRS rates were significantly lower in cohort 1 (38.1%, n=8) versus cohort 2 (75%, n=15, p=0.03). Grade 2 CRS occurred in 4.8% (n=1) of patients in cohort 1 and 19% (n=4) of patients in cohort 2 (p=0.09). CRS events occurred following the first step-up dose in 5/21 and 10/20 patients in cohort 1 and 2, respectively. In univariate logistic regression analysis, no prior exposure to TCRT was associated with about a 5-fold increase in the incidence of CRS with Tec (95% CI: 1.3-20.2, p=0.042). After adjusting for age, EMD and elevated LDH levels, the impact of prior exposure to TCRT remained significant with an odds ratio of 4.5 (95% CI: 1.1-20.6, p=0.01).
Conclusions: In our study cohorts, prior exposure to a TCRT was associated with a significantly lower incidence of CRS during Tec step-up dosing phase. This observation will allow for optimization of CRS prophylactic strategies for RRMM patients.
Methods: Our institutional plasma cell disorders database was queried to identify RRMM patients who received commercial Tec from November 2022 to May 2023. Patients who completed the step-up dosing phase (first step-up, second step-up and first full doses) were divided into two cohorts based on TCRT exposure before Tec (prior TCRT exposure: cohort 1 and no prior TCRT exposure: cohort 2). Data collection included patient demographics, disease characteristics, prior LOT, and rates/grades of CRS and ICANS. The Chi-square/Fisher exact test was used to compare differences in CRS rates between the two cohorts. Univariate and multivariate logistic regression analyses were performed to assess impact of prior TCRT exposure on CRS rates with Tec. Statistical analysis was performed using SPSS software (version 29).
Results: 41 patients (cohort 1: 21 and cohort 2: 20) were included in the final analysis. Baseline characteristics were comparable between the two cohorts except for previous LOT: 8 (range: 4-13) in cohort 1 and 6 (range: 3-15) in cohort 2 (p=0.02). High-risk cytogenetic abnormalities [t (4;14), t (14;16), t (14;20), TP53 mutations, del 17p and 1q amplification) were present in 71% (n=15) and 40% (n=8) of patients in cohorts 1 and 2, respectively (p=0.06). Extramedullary disease (EMD) was present in 57% (n=12) of patients in cohort 1 and 50% (n=10) in cohort 2. Elevated LDH (prior to teclistamab) was seen in 33% (n=7) of patients in cohort 1 and 15% (n=3) in cohort 2 (p=0.27). CRS rates were significantly lower in cohort 1 (38.1%, n=8) versus cohort 2 (75%, n=15, p=0.03). Grade 2 CRS occurred in 4.8% (n=1) of patients in cohort 1 and 19% (n=4) of patients in cohort 2 (p=0.09). CRS events occurred following the first step-up dose in 5/21 and 10/20 patients in cohort 1 and 2, respectively. In univariate logistic regression analysis, no prior exposure to TCRT was associated with about a 5-fold increase in the incidence of CRS with Tec (95% CI: 1.3-20.2, p=0.042). After adjusting for age, EMD and elevated LDH levels, the impact of prior exposure to TCRT remained significant with an odds ratio of 4.5 (95% CI: 1.1-20.6, p=0.01).
Conclusions: In our study cohorts, prior exposure to a TCRT was associated with a significantly lower incidence of CRS during Tec step-up dosing phase. This observation will allow for optimization of CRS prophylactic strategies for RRMM patients.
