Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-492: Pharmacodynamic Effects of Tiragolumab, as Monotherapy and In Combos with Daratumumab and Atezolizumab in Patients with R/R MM: Biomarker Results From a Phase 1a/1b Trial
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST

Shannon Moore, PhD (they/them/theirs)
Principal Scientist
Genentech, Inc., South San Francisco, CA, USA
South San Francisco, California, United States
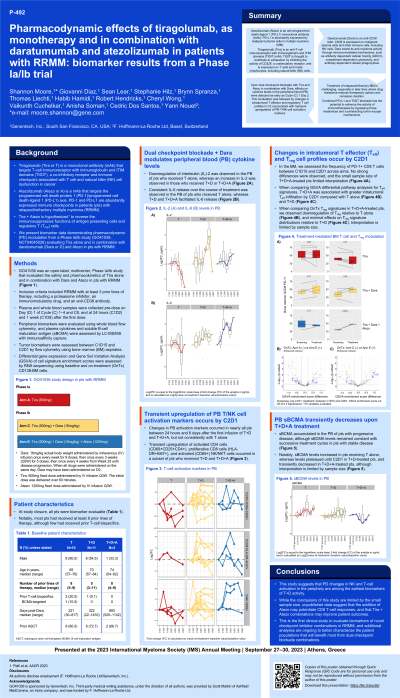
Introduction: Tiragolumab (Tira) is a monoclonal antibody (mab) that targets TIGIT, a co-inhibitory receptor and immune checkpoint associated with T cell and natural killer cell (NK) dysfunction in cancer. Atezolizumab (Atezo) is a mab that targets the PD-1/PD-L1 axis, abundantly expressed immune checkpoints in Relapsed/Refractory (R/R) Multiple Myeloma (MM) patients (pts). Tira + Atezo administration is intended to reverse immunosuppressive functions of antigen presenting cells and regulatory T cells. Here we present biomarker data demonstrating pharmacodynamic modulation in a Phase Ia/Ib study (GO41036; NCT04045028) evaluating Tira alone (n=10), Tira with Daratumumab (Dara) (T+D) (n=11), or Tira with Dara and Atezo (T+D+A) (n=3) in R/R MM pts.
Methods: Peripheral biomarkers were evaluated using whole blood flow cytometry, plasma cytokine, and soluble BCMA (sBCMA) by LC-MS/MS with immunoaffinity capture. Tumor biomarkers were assessed by flow cytometry using bone marrow (BM) aspirates. Differential gene expression and Gene Set Variation Analysis of cell signature enrichment scores were assessed by RNAseq using baseline and on-treatment CD138- BM cells.
Results: In peripheral blood (PB), sBCMA accumulated in pts with progressive disease, though levels remained constant with successive treatment cycles in pts with stable disease. Changes in PB activation markers occurred between 24h and 8d after first infusion, though were not observed in Tira mono treated pts. Transient upregulation of CD69+CD25+ CD4 T cells occurred in a subset of T+D treated pts, while a trend of NK/NKT CD69 upregulation was observed earlier and at a greater magnitude in two of three T+D+A treated pts when compared to T+D. Notably, NK absolute counts decreased by C1D8 in combination arms, consistent with Dara-mediated effects. Frequencies of PB Ki-67+HLA-DR+ CD8 T cells were transiently upregulated by C1D8 in pts receiving T+D+A, and in a subset of T+D treated pts. In the BM, the frequency of PD-1+ CD8 T cells significantly increased between C1D15 and C2D1 in T+D and to a greater extent in T+D+A treated pts. Additional transcriptomic analysis to interrogate modulation of gene expressions and cell signatures over treatment is ongoing, however, initial reports suggest T+D treatment significantly increased NK, CD8 T cell, and macrophage signatures within the BM, but this was not observed with Tira alone.
Conclusions: The study demonstrated that PD changes in NK and T cell activation in the periphery are among the earliest biomarkers of T+D activity, and that the addition of Atezo may potentiate CD8 T cell responses, suggesting that Tira + Atezo combinations may improve pt outcomes. This is the first clinical study to evaluate biomarkers of novel checkpoint inhibitor combinations in R/R MM, and additional analyses are ongoing to better characterize patient populations that will benefit most from dual checkpoint blockade combinations.
Methods: Peripheral biomarkers were evaluated using whole blood flow cytometry, plasma cytokine, and soluble BCMA (sBCMA) by LC-MS/MS with immunoaffinity capture. Tumor biomarkers were assessed by flow cytometry using bone marrow (BM) aspirates. Differential gene expression and Gene Set Variation Analysis of cell signature enrichment scores were assessed by RNAseq using baseline and on-treatment CD138- BM cells.
Results: In peripheral blood (PB), sBCMA accumulated in pts with progressive disease, though levels remained constant with successive treatment cycles in pts with stable disease. Changes in PB activation markers occurred between 24h and 8d after first infusion, though were not observed in Tira mono treated pts. Transient upregulation of CD69+CD25+ CD4 T cells occurred in a subset of T+D treated pts, while a trend of NK/NKT CD69 upregulation was observed earlier and at a greater magnitude in two of three T+D+A treated pts when compared to T+D. Notably, NK absolute counts decreased by C1D8 in combination arms, consistent with Dara-mediated effects. Frequencies of PB Ki-67+HLA-DR+ CD8 T cells were transiently upregulated by C1D8 in pts receiving T+D+A, and in a subset of T+D treated pts. In the BM, the frequency of PD-1+ CD8 T cells significantly increased between C1D15 and C2D1 in T+D and to a greater extent in T+D+A treated pts. Additional transcriptomic analysis to interrogate modulation of gene expressions and cell signatures over treatment is ongoing, however, initial reports suggest T+D treatment significantly increased NK, CD8 T cell, and macrophage signatures within the BM, but this was not observed with Tira alone.
Conclusions: The study demonstrated that PD changes in NK and T cell activation in the periphery are among the earliest biomarkers of T+D activity, and that the addition of Atezo may potentiate CD8 T cell responses, suggesting that Tira + Atezo combinations may improve pt outcomes. This is the first clinical study to evaluate biomarkers of novel checkpoint inhibitor combinations in R/R MM, and additional analyses are ongoing to better characterize patient populations that will benefit most from dual checkpoint blockade combinations.
