Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-233: Physician perspectives regarding conventional marrow testing and MRD assessments to guide decision-making in myeloma
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST

Rahul Banerjee, MD
Assistant Professor, Clinical Research Division
Fred Hutchinson Cancer Center
Seattle, Washington, United States
Introduction:
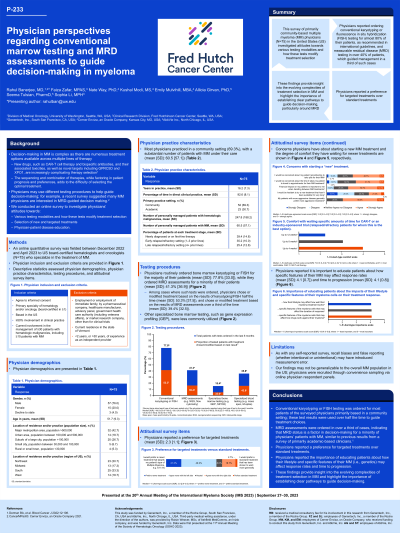
Background: Decision-making in multiple myeloma (MM) is complex as there are numerous treatment options available across multiple lines of therapy. A recent survey suggested many MM physicians are interested in MRD-guided decision making (Derman et al., 2022). We thus conducted an online survey to investigate physicians’ attitudes toward MRD assessments and conventional marrow testing (e.g., FISH or karyotyping) and how these tests modify treatment selection.
Methods:
Methods: Board-certified hematologists and/or oncologists (N=75) who had ≥10 patients with MM, spent ≥50% of time in clinical practice in the US, and had been in clinical practice for at least two years completed an online survey. Descriptive statistics assessed practice characteristics, testing procedures, and attitudinal items.
Results:
Results: Most physicians practiced in a community setting (69%) with a substantial number of MM patients under their care (M=60.5, SD=57.1, Mdn=40.0, IQR 25-75). Most physicians routinely ordered bone marrow karyotyping or FISH (M=77.8%, SD=33.0, Mdn=100.0%, IQR 50-100%), while a significant minority routinely ordered MRD assessments (M=41.3%, SD=36.9, Mdn=30.0%, IQR 10-80%). Among cases where such tests were ordered, physicians chose or modified treatment based on the results of karyotyping/FISH half the time (M=53.3%, SD=37.5, Mdn=50.0%, IQR 23-100%) and chose or modified treatment based on the results of MRD assessments only a third of the time (M=39.4%, SD=32.5, Mdn=30.0%, IQR 10-60%). On an agreement scale anchored at 1 (prefer personalized treatment approaches) versus 5 (prefer standard treatment approaches that consistently work), physicians reported a slight preference for targeted treatments (M=2.3, SD=1.1, Mdn=2.0, IQR 2-3). On a 1-5 Likert-type agreement scale, physicians reported it is important to educate patients about how specific features of their MM may affect response rates (M=4.1, SD=0.7, Mdn=4.0, IQR 4-5) and time to progression (M=4.1, SD=0.8, Mdn=4.0, IQR 4-5).
Conclusions:
Conclusions: In our study of physicians primarily based in a community setting, most ordered conventional karyotyping or FISH testing for their patients and utilized these test results to guide treatment choices. MRD assessments were ordered in a third of cases and used to guide management in a third of cases when ordered. These findings highlight the importance of establishing clear pathways to guide decision-making in MM.
Background: Decision-making in multiple myeloma (MM) is complex as there are numerous treatment options available across multiple lines of therapy. A recent survey suggested many MM physicians are interested in MRD-guided decision making (Derman et al., 2022). We thus conducted an online survey to investigate physicians’ attitudes toward MRD assessments and conventional marrow testing (e.g., FISH or karyotyping) and how these tests modify treatment selection.
Methods:
Methods: Board-certified hematologists and/or oncologists (N=75) who had ≥10 patients with MM, spent ≥50% of time in clinical practice in the US, and had been in clinical practice for at least two years completed an online survey. Descriptive statistics assessed practice characteristics, testing procedures, and attitudinal items.
Results:
Results: Most physicians practiced in a community setting (69%) with a substantial number of MM patients under their care (M=60.5, SD=57.1, Mdn=40.0, IQR 25-75). Most physicians routinely ordered bone marrow karyotyping or FISH (M=77.8%, SD=33.0, Mdn=100.0%, IQR 50-100%), while a significant minority routinely ordered MRD assessments (M=41.3%, SD=36.9, Mdn=30.0%, IQR 10-80%). Among cases where such tests were ordered, physicians chose or modified treatment based on the results of karyotyping/FISH half the time (M=53.3%, SD=37.5, Mdn=50.0%, IQR 23-100%) and chose or modified treatment based on the results of MRD assessments only a third of the time (M=39.4%, SD=32.5, Mdn=30.0%, IQR 10-60%). On an agreement scale anchored at 1 (prefer personalized treatment approaches) versus 5 (prefer standard treatment approaches that consistently work), physicians reported a slight preference for targeted treatments (M=2.3, SD=1.1, Mdn=2.0, IQR 2-3). On a 1-5 Likert-type agreement scale, physicians reported it is important to educate patients about how specific features of their MM may affect response rates (M=4.1, SD=0.7, Mdn=4.0, IQR 4-5) and time to progression (M=4.1, SD=0.8, Mdn=4.0, IQR 4-5).
Conclusions:
Conclusions: In our study of physicians primarily based in a community setting, most ordered conventional karyotyping or FISH testing for their patients and utilized these test results to guide treatment choices. MRD assessments were ordered in a third of cases and used to guide management in a third of cases when ordered. These findings highlight the importance of establishing clear pathways to guide decision-making in MM.
