Cellular and T cell engager Immunotherapy
Poster Session 1
P-048: POINT-OF-CARE ANTI-BCMA CAR T-CELL THERAPY INDUCES ENCOURAGING RESPONSE RATES IN RELAPSED/REFRACTORY MULTIPLE MYELOMA PATIENTS MOSTLY WITH HIGH-RISK DISEASE FEATURES
Wednesday, September 27, 2023
1:30 PM - 2:30 PM EEST

Eden Shkury
Medical intern, Division of Hematology and Bone Marrow Transplantation
Chaim Sheba Medical Center, Israel
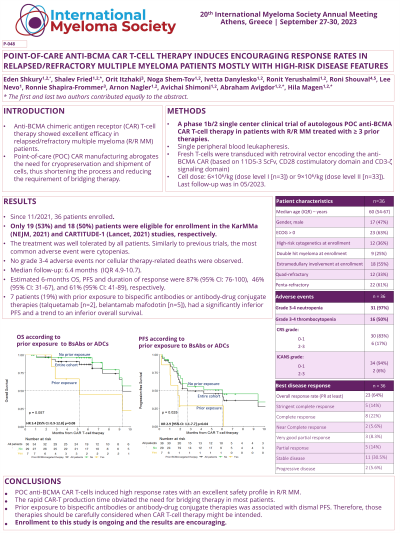
Introduction: Anti-BCMA chimeric antigen receptor (CAR) T-cell therapy showed excellent efficacy in relapsed/refractory multiple myeloma (R/R MM) patients (pts). Point-of-care (POC) CAR manufacturing abrogates the need for cryopreservation and shipment of cells, thus shortening the manufacturing process and reducing the necessity of bridging therapy. We report outcomes of phase 1b/2 single center clinical trial of autologous POC anti-BCMA CAR T-cell therapy in pts with R/R MM treated with ≥ 3 prior therapies.
Methods: Pts underwent a single peripheral blood leukapheresis. Fresh T-cells were transduced with retroviral vector encoding the anti-BCMA CAR (based on 11D5-3 ScFv, CD28 costimulatory domain and CD3-ζ signaling domain). Cell dose was 6×10^6/kg (dose level I [n=3]) or 9×10^6/kg (dose level II [n=33]). Primary endpoints were overall response rate (ORR) per IMWG criteria and safety. Secondary endpoints were overall survival (OS) and progression-free survival (PFS). Last follow-up was 05/2023.
Results: Since 11/2021, 36 pts enrolled (median age 60, IQR 54-67). All pts received CAR T-cell infusion in a median of 11 days (IQR 11-14) after leukapheresis. Only 2 pts received bridging therapy. The median number of prior therapies was 4 (IQR 3-5), with 61% and 33% of the pts being penta and quad-refractory, respectively. 7 (19%) pts had prior exposure to BCMA-targeted therapy (belantamab mafodotin, n=5 [14%]; talqeutamab, n=2 [6%]). At enrollment, 12 (33%) pts had high-risk cytogenetics, 9 (25%) had double-hit myeloma, and 18 (50%) had extramedullary involvement. Only 19 (53%) and 18 (50%) pts were eligible to enroll in the KarMMa (NEJM, 2021) and CARTITUDE-1 (Lancet, 2021) studies, respectively.
Only 1 patient (3%) developed grade ≥ 3 cytokine release syndrome, and 1 patient (3%) developed grade ≥ 3 immune effector cell-associated neurotoxicity syndrome. Grade 3-4 neutropenia and thrombocytopenia occurred in 35 (97%) and 19 (53%) pts, respectively. Anemia requiring transfusion occurred in 17 (47%) pts. No grade 3-4 adverse events nor cellular therapy-related deaths were observed.
The median follow-up was 6.4 months (IQR 4.9-10.7). Best ORR (PR at least) was 64% (VGPR at least, 50%). Median time to first response was 31 days (95% CI: 26-33). Estimated 6-months OS, PFS and duration of response were 87% (95% CI: 76-100), 46% (95% CI: 31-67), and 61% (95% CI: 41-89), respectively. Pts with prior exposure to BCMA-targeted therapies had an inferior PFS (HR 2.9 [95% CI: 1.1-7.8] p=0.04).
Conclusions: POC anti-BCMA CAR T-cells induced high response rates with an excellent safety profile in R/R MM pts mostly not eligible to be enrolled in the pivotal trials. The rapid CAR-T production time obviated the need for bridging therapy in most pts. It is noteworthy that prior exposure to BCMA-targeted therapies is associated with dismal PFS, hence those therapies should be carefully considered when CAR T-cell therapy might be intended.
Methods: Pts underwent a single peripheral blood leukapheresis. Fresh T-cells were transduced with retroviral vector encoding the anti-BCMA CAR (based on 11D5-3 ScFv, CD28 costimulatory domain and CD3-ζ signaling domain). Cell dose was 6×10^6/kg (dose level I [n=3]) or 9×10^6/kg (dose level II [n=33]). Primary endpoints were overall response rate (ORR) per IMWG criteria and safety. Secondary endpoints were overall survival (OS) and progression-free survival (PFS). Last follow-up was 05/2023.
Results: Since 11/2021, 36 pts enrolled (median age 60, IQR 54-67). All pts received CAR T-cell infusion in a median of 11 days (IQR 11-14) after leukapheresis. Only 2 pts received bridging therapy. The median number of prior therapies was 4 (IQR 3-5), with 61% and 33% of the pts being penta and quad-refractory, respectively. 7 (19%) pts had prior exposure to BCMA-targeted therapy (belantamab mafodotin, n=5 [14%]; talqeutamab, n=2 [6%]). At enrollment, 12 (33%) pts had high-risk cytogenetics, 9 (25%) had double-hit myeloma, and 18 (50%) had extramedullary involvement. Only 19 (53%) and 18 (50%) pts were eligible to enroll in the KarMMa (NEJM, 2021) and CARTITUDE-1 (Lancet, 2021) studies, respectively.
Only 1 patient (3%) developed grade ≥ 3 cytokine release syndrome, and 1 patient (3%) developed grade ≥ 3 immune effector cell-associated neurotoxicity syndrome. Grade 3-4 neutropenia and thrombocytopenia occurred in 35 (97%) and 19 (53%) pts, respectively. Anemia requiring transfusion occurred in 17 (47%) pts. No grade 3-4 adverse events nor cellular therapy-related deaths were observed.
The median follow-up was 6.4 months (IQR 4.9-10.7). Best ORR (PR at least) was 64% (VGPR at least, 50%). Median time to first response was 31 days (95% CI: 26-33). Estimated 6-months OS, PFS and duration of response were 87% (95% CI: 76-100), 46% (95% CI: 31-67), and 61% (95% CI: 41-89), respectively. Pts with prior exposure to BCMA-targeted therapies had an inferior PFS (HR 2.9 [95% CI: 1.1-7.8] p=0.04).
Conclusions: POC anti-BCMA CAR T-cells induced high response rates with an excellent safety profile in R/R MM pts mostly not eligible to be enrolled in the pivotal trials. The rapid CAR-T production time obviated the need for bridging therapy in most pts. It is noteworthy that prior exposure to BCMA-targeted therapies is associated with dismal PFS, hence those therapies should be carefully considered when CAR T-cell therapy might be intended.
