Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-230: Pomalidomide, daratumumab, and dexamethasone after lenalidomide treatment in patients with relapsed or refractory multiple myeloma (RRMM): final overall survival analysis of the phase 2 MM-014 study
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST

Nizar J. Bahlis, MD
Associate Professor of Medicine - Hematology and Bone Marrow Transplantation
Arnie Charbonneau Cancer Institute - University of Calgary
Calgary, Alberta, Canada
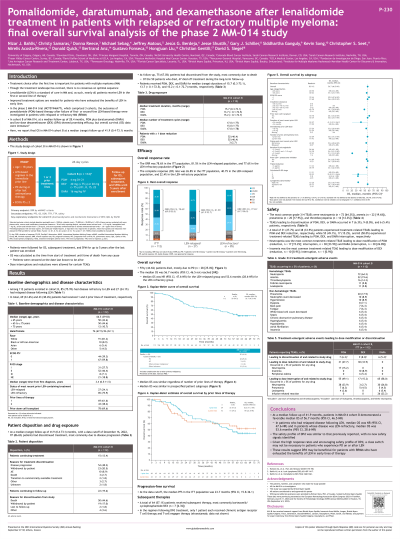
Introduction: Nearly all patients (pts) with multiple myeloma (MM) receive lenalidomide (LEN) in first or second line of treatment (tx; LoT). Pts with RRMM who have exhausted LEN benefits need improved options. The phase 2 MM-014 trial (NCT01946477) explored pomalidomide (POM)-based tx in early LoT for RRMM in 3 cohorts. In cohort B, at a median follow-up of 28.4mo, POM+daratumumab (DARA)+low-dose dexamethasone (DEX; DPd) showed promising efficacy, with an overall response rate (ORR) of 77.7% and median progression-free survival of 30.8mo (Bahlis, Leuk Lymphoma 2022). Here, we report the final overall survival (OS) in this cohort.
Methods: In cohort B, pts aged ≥18y with RRMM who had received 1–2 prior LoT with LEN-based regimen as their most recent were eligible. Pts received DPd in 28-d cycles (C): POM 4mg orally on d1–21; DEX 40mg (age ≤75y) or 20mg (age >75y) orally on d1, 8, 15, 22; DARA intravenously 16 mg/kg bodyweight on d1, 8, 15, 22 of C1–2, d1, 5 of C3–6, and d1 of C7 and beyond. ORR was the primary endpoint; OS and safety were secondary endpoints. OS was defined as time from tx start to time of death from any cause; pts were censored at date last known to be alive. Dose interruptions and reductions were allowed for certain tx-emergent adverse events (TEAEs). Pts were followed for OS, subsequent tx, and second primary malignancies for ≤5y after last pt was enrolled.
Results: Among 112 pts enrolled, 85 (75.9%) had LEN-refractory disease and 27 (24.1%) had LEN-relapsed disease; 69 (61.6%) and 43 (38.4%) received 1 and 2 prior LoT, respectively. At a median (range) follow-up of 41.9 (0.4–73.1) mo, 96 (85.7%) pts had discontinued tx, 54 (48.2%) due to progressive disease (PD). Pts received POM, DEX, and DARA for median (range) durations of 15.7 (0.3–73.1), 13.7 ( < 0.1–72.5), and 15.2 ( < 0.1–72.7) mo, respectively. Fifty (44.6%) pts died, mostly due to PD (n=28 [25.0%]). Median (95% CI) OS was 56.7 mo (46.5–not reached [NR]): 53.6 mo (28.6–NR) and NR (47.6–NR) for pts who had LEN-refractory and LEN-relapsed disease, respectively. TEAEs leading to POM, DEX, or DARA discontinuation occurred in 7 (6.3%), 9 (8.0%), and 6 (5.4%) pts, respectively. Tx-related TEAEs led to POM and DEX reduction in 31 (27.7%) and 38 (33.9%) pts, respectively; and led to POM, DEX, and DARA interruption in 55 (49.1%), 17 (15.2%), and 65 (58.0%) pts, respectively. Neutropenia was the most common tx-related TEAE leading to dose modification of POM (reduction, n=17 [15.2%]; interruption, n=38 [33.9%]) and DARA (interruption, n=30 [26.8%]); insomnia was the most common tx-related TEAE leading to DEX dose modification (reduction, n=10 [8.9%]; interruption, n=1 [0.9%]).
Conclusions: With long-term follow-up, pts with RRMM treated with DPd showed favorable OS. The DPd safety profile was similar to previous reports, with no new safety signals identified. These data suggest that DPd is beneficial for pts with RRMM who have exhausted benefits of LEN.
Presented at EHA 2023. Abstract P882 (https://library.ehaweb.org/).
Methods: In cohort B, pts aged ≥18y with RRMM who had received 1–2 prior LoT with LEN-based regimen as their most recent were eligible. Pts received DPd in 28-d cycles (C): POM 4mg orally on d1–21; DEX 40mg (age ≤75y) or 20mg (age >75y) orally on d1, 8, 15, 22; DARA intravenously 16 mg/kg bodyweight on d1, 8, 15, 22 of C1–2, d1, 5 of C3–6, and d1 of C7 and beyond. ORR was the primary endpoint; OS and safety were secondary endpoints. OS was defined as time from tx start to time of death from any cause; pts were censored at date last known to be alive. Dose interruptions and reductions were allowed for certain tx-emergent adverse events (TEAEs). Pts were followed for OS, subsequent tx, and second primary malignancies for ≤5y after last pt was enrolled.
Results: Among 112 pts enrolled, 85 (75.9%) had LEN-refractory disease and 27 (24.1%) had LEN-relapsed disease; 69 (61.6%) and 43 (38.4%) received 1 and 2 prior LoT, respectively. At a median (range) follow-up of 41.9 (0.4–73.1) mo, 96 (85.7%) pts had discontinued tx, 54 (48.2%) due to progressive disease (PD). Pts received POM, DEX, and DARA for median (range) durations of 15.7 (0.3–73.1), 13.7 ( < 0.1–72.5), and 15.2 ( < 0.1–72.7) mo, respectively. Fifty (44.6%) pts died, mostly due to PD (n=28 [25.0%]). Median (95% CI) OS was 56.7 mo (46.5–not reached [NR]): 53.6 mo (28.6–NR) and NR (47.6–NR) for pts who had LEN-refractory and LEN-relapsed disease, respectively. TEAEs leading to POM, DEX, or DARA discontinuation occurred in 7 (6.3%), 9 (8.0%), and 6 (5.4%) pts, respectively. Tx-related TEAEs led to POM and DEX reduction in 31 (27.7%) and 38 (33.9%) pts, respectively; and led to POM, DEX, and DARA interruption in 55 (49.1%), 17 (15.2%), and 65 (58.0%) pts, respectively. Neutropenia was the most common tx-related TEAE leading to dose modification of POM (reduction, n=17 [15.2%]; interruption, n=38 [33.9%]) and DARA (interruption, n=30 [26.8%]); insomnia was the most common tx-related TEAE leading to DEX dose modification (reduction, n=10 [8.9%]; interruption, n=1 [0.9%]).
Conclusions: With long-term follow-up, pts with RRMM treated with DPd showed favorable OS. The DPd safety profile was similar to previous reports, with no new safety signals identified. These data suggest that DPd is beneficial for pts with RRMM who have exhausted benefits of LEN.
Presented at EHA 2023. Abstract P882 (https://library.ehaweb.org/).
