Treatment of Newly Diagnosed Myeloma - Transplant Eligible
Poster Session 1
P-132: Post-induction Undetectable Flow Minimal Residual Disease ameliorates the high risk determined by FISH among Newly Diagnosed Multiple Myeloma
Wednesday, September 27, 2023
1:30 PM - 2:30 PM EEST

Guldane Cengiz Seval, MD
Assoc. Prof.
Ankara University School of Medicine, Department of Hematology, Ankara, Turkey
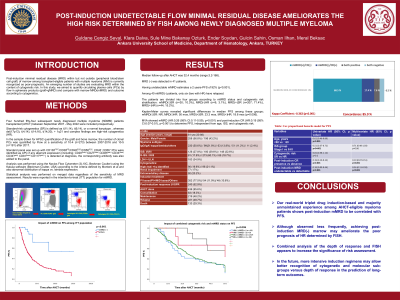
Introduction: Post-induction minimal residual disease(MRD) within marrow is currently recognized as poor-prognostic among transplant-eligible patients with multiple myeloma(MM). An emerging number of studies are evaluating MRD within the context of cytogenetic risk. In this study, we aimed to quantify clonal plasma cells (PCs) by flow both in apheresis products(gMRD) and marrow(mMRD) to evaluate the impact on the outcome according to risk determined by FISH cytogenetics.
Methods: Four hundred fifty-four subsequent newly diagnosed MM patients transplanted between 2007-2022 were included prospectively. Standard-risk cytogenetics(SR) is defined as t(11;14) or a normal karyotype , whereas del(17p13), t(4;14), t(14;16), + 1q21 and complex findings are high-risk cytogenetics(HR).Results were reported in the intention-to-treat(ITT) population for mMRD.
Results: Median follow-up after AHCT was 32.4 mos(range:3.2-168). The induction regimen consisted of bortezomib without or with immunomodulatory drugs 77.5% and 11.9%. Consolidation 19%(n=83/437), and maintenance 27.4%(n=118/431) were administered based on the guidelines and regulations. Cytogenetically HR, standard or missing were observed in 18.5%(n=84), 77.5%(n=352) and 4%(n=18) of the total cohort. Post-induction complete response(CR) was achieved in 18.7% of patients(n=85). Following mobilization(n=453), gMRD and mMRD were undetectable in 48.9%(181/370) and 13.5%(41/303) of patients. There was a correlation between gMRD and mMRD(SE: 0.318, p< 0.001). Having undetectable mMRD estimates a 5 years-PFS of 71.3% (p < 0.001). Among 40 mMRD(-) patients, only six (two with HR) have relapsed. Likewise, 5 years-PFS according to undetectable gMRD 44.8% (p=0.02) or according to HR vs SR is 31.3% vs 37.8% (p=0.19). Distribution of patients divided into four groups according to mMRD status and cytogenetic risk are as follows: mMRD(-)SR (n=30; 10.3%), MRD(-)HR (n=9; 3.1%), MRD(+)SR (n=207; 71.4%), MRD(+)HR (n=44;15.2%). Kaplan-Meier curves revealed significant differences in median PFS among these groups; mMRD(-)SR: NR, MRD(-)HR: 50 mos, MRD(+)SR: 23.3 mos, MRD(+)HR: 18.6 mos (p=0.006). In a MVA model (age, ISS, FISH, post-induction CR or MRD) post-induction mMRD (HR:0.26 (95% CI:0.11-0.59),p < 0.001) and post-induction CR (HR:0.19 (95% CI:0.07-0.51),p < 0.001) appeared to determine PFS independently.
Conclusions: Our real-world triplet drug induction-based and majority unmaintained experience among AHCT-eligible myeloma patients, shows post-induction mMRD to be correlated with PFS. Although observed less frequently, achieving post-induction MRD(-) marrow may ameliorate the poor prognosis of HR determined by FISH. Combined analysis of the depth of response and FISH appears to increase the significance of risk assessment. In the future, more intensive induction regimens may allow better recognition of cytogenetic and molecular sub-groups versus depth of response in the prediction of long-term outcomes.
Methods: Four hundred fifty-four subsequent newly diagnosed MM patients transplanted between 2007-2022 were included prospectively. Standard-risk cytogenetics(SR) is defined as t(11;14) or a normal karyotype , whereas del(17p13), t(4;14), t(14;16), + 1q21 and complex findings are high-risk cytogenetics(HR).Results were reported in the intention-to-treat(ITT) population for mMRD.
Results: Median follow-up after AHCT was 32.4 mos(range:3.2-168). The induction regimen consisted of bortezomib without or with immunomodulatory drugs 77.5% and 11.9%. Consolidation 19%(n=83/437), and maintenance 27.4%(n=118/431) were administered based on the guidelines and regulations. Cytogenetically HR, standard or missing were observed in 18.5%(n=84), 77.5%(n=352) and 4%(n=18) of the total cohort. Post-induction complete response(CR) was achieved in 18.7% of patients(n=85). Following mobilization(n=453), gMRD and mMRD were undetectable in 48.9%(181/370) and 13.5%(41/303) of patients. There was a correlation between gMRD and mMRD(SE: 0.318, p< 0.001). Having undetectable mMRD estimates a 5 years-PFS of 71.3% (p < 0.001). Among 40 mMRD(-) patients, only six (two with HR) have relapsed. Likewise, 5 years-PFS according to undetectable gMRD 44.8% (p=0.02) or according to HR vs SR is 31.3% vs 37.8% (p=0.19). Distribution of patients divided into four groups according to mMRD status and cytogenetic risk are as follows: mMRD(-)SR (n=30; 10.3%), MRD(-)HR (n=9; 3.1%), MRD(+)SR (n=207; 71.4%), MRD(+)HR (n=44;15.2%). Kaplan-Meier curves revealed significant differences in median PFS among these groups; mMRD(-)SR: NR, MRD(-)HR: 50 mos, MRD(+)SR: 23.3 mos, MRD(+)HR: 18.6 mos (p=0.006). In a MVA model (age, ISS, FISH, post-induction CR or MRD) post-induction mMRD (HR:0.26 (95% CI:0.11-0.59),p < 0.001) and post-induction CR (HR:0.19 (95% CI:0.07-0.51),p < 0.001) appeared to determine PFS independently.
Conclusions: Our real-world triplet drug induction-based and majority unmaintained experience among AHCT-eligible myeloma patients, shows post-induction mMRD to be correlated with PFS. Although observed less frequently, achieving post-induction MRD(-) marrow may ameliorate the poor prognosis of HR determined by FISH. Combined analysis of the depth of response and FISH appears to increase the significance of risk assessment. In the future, more intensive induction regimens may allow better recognition of cytogenetic and molecular sub-groups versus depth of response in the prediction of long-term outcomes.
