QoL and Patient-Reported Outcome and Supportive Care
Poster Session 3
P-453: Randomized Phase II Study of Digital Life Coaching during Stem Cell Transplantation for Myeloma
Friday, September 29, 2023
1:15 PM - 2:15 PM EEST

Rahul Banerjee, MD
Assistant Professor, Clinical Research Division
Fred Hutchinson Cancer Center
Seattle, Washington, United States
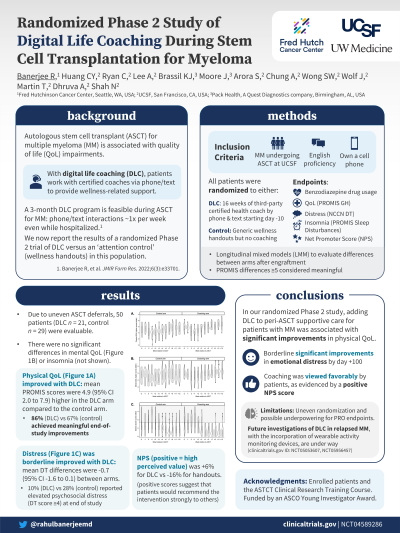
Introduction: Autologous stem cell transplantation (ASCT) for multiple myeloma (MM) is associated with quality of life (QOL) impairments that may lead to long-term psychosocial issues or premature workforce retirement. Our pilot study previously demonstrated the feasibility of digital life coaching (DLC), whereby certified coaches work with patients via phone/text to provide wellness-related support during the peri-ASCT period. We now report the results of a randomized Phase II trial of DLC (clinicaltrials.gov ID NCT04589286) in this population.
Methods: English-speaking patients with MM who owned cellphones were randomized to wellness handouts (control) versus an additional 16-week coaching subscription (DLC) beginning at Day -10. Endpoints included benzodiazepine or zolpidem-drug (B/Z) medication use, physical/mental QOL (PROMIS Global Health), distress (Distress Thermometer), insomnia (PROMIS Sleep Disturbances 4A), and Likert scales regarding study interventions. Linear mixed-effect modeling (LMM) was used to compare patient-reported endpoints.
Results: Due to uneven rates of post-enrollment ASCT deferrals, 50 patients (coaching n = 21, control n = 29) were evaluable. Baseline characteristics, B/Z use, mental QOL, and insomnia were similar between arms apart from age (medians 68 in the DLC arm vs 61 in the control arm, p< 0.01). Physical QOL was improved with coaching (mean LMM difference +4.9, 95% CI +2.0 to +7.9); 86% versus 67% of patients achieved a meaningful physical QOL improvement at study conclusion compared to engraftment (≥5 points). Distress was borderline improved as well (mean LMM difference -0.7 points, 95% CI -1.6 to +0.1); for example, 10% (DLC) versus 28% (control) reported elevated distress (≥4) at the final assessment. Net Promoter Scores (with positive scores indicating high perceived value by patients) were -16% for handouts and +6% for DLC.
Conclusions: Although limited by underpowering and global reductions in B/Z use compared to our historical data, our study demonstrated that DLC during ASCT was associated with improved physical QOL and a clear trend toward lower levels of distress. Future investigations of DLC in other oncologic settings, including relapsed MM, are under way.
Methods: English-speaking patients with MM who owned cellphones were randomized to wellness handouts (control) versus an additional 16-week coaching subscription (DLC) beginning at Day -10. Endpoints included benzodiazepine or zolpidem-drug (B/Z) medication use, physical/mental QOL (PROMIS Global Health), distress (Distress Thermometer), insomnia (PROMIS Sleep Disturbances 4A), and Likert scales regarding study interventions. Linear mixed-effect modeling (LMM) was used to compare patient-reported endpoints.
Results: Due to uneven rates of post-enrollment ASCT deferrals, 50 patients (coaching n = 21, control n = 29) were evaluable. Baseline characteristics, B/Z use, mental QOL, and insomnia were similar between arms apart from age (medians 68 in the DLC arm vs 61 in the control arm, p< 0.01). Physical QOL was improved with coaching (mean LMM difference +4.9, 95% CI +2.0 to +7.9); 86% versus 67% of patients achieved a meaningful physical QOL improvement at study conclusion compared to engraftment (≥5 points). Distress was borderline improved as well (mean LMM difference -0.7 points, 95% CI -1.6 to +0.1); for example, 10% (DLC) versus 28% (control) reported elevated distress (≥4) at the final assessment. Net Promoter Scores (with positive scores indicating high perceived value by patients) were -16% for handouts and +6% for DLC.
Conclusions: Although limited by underpowering and global reductions in B/Z use compared to our historical data, our study demonstrated that DLC during ASCT was associated with improved physical QOL and a clear trend toward lower levels of distress. Future investigations of DLC in other oncologic settings, including relapsed MM, are under way.
