Myeloma Microenvironment and immune profiling
Poster Session 3
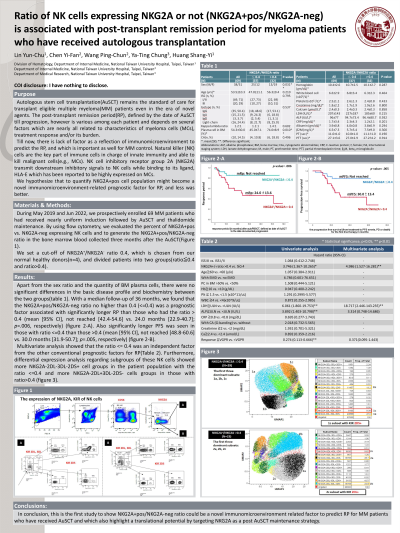
P-491: Ratio of NK cells expressingNKG2A or not (NKG2A+pos/NKG2A-neg) is associated with post-transplant remission period for myeloma patients who have received autologous transplantation
Friday, September 29, 2023
1:15 PM - 2:15 PM EEST
Yun-chu Lin, MD
Attending
National Taiwan University Hospital, Taiwan (Republic of China)
Introduction: Autologous stem cell transplantation (AuSCT) remains the standard of care for transplant eligible multiple myeloma (MM) patients even in the era of novel agents. The post-transplant remission period (RP), defined by the date of AuSCT till progression, however is various among each patient and depends on several factors which are nearly all related to characteristics of myeloma cells (MCs), treatment response and/or its burden. Till now, there is lack of factor as a reflection of immunomicroenvironment to predict the RP, and which is important as well for MM control. Natural killer (NK) cells are the key part of immune cells in charge of innate immunity and able to kill malignant cells (e.g., MCs). NK cell inhibitory receptor group 2A (NKG2A) transmit downstream inhibitory signals to NK cells while binding to its ligand, HLA-E which has been reported to be highly expressed on MCs. We hypothesize that to quantify NKG2A+pos cell population might become a novel immunomicroenvironment related prognostic factor for RP, and less was better.
Methods: During May 2019 and Jun 2022, we prospectively enrolled 69 MM patients who had received nearly uniform induction followed by AuSCT and thalidomide maintenance. By using flow cytometry, we evaluated the percent of NKG2A+pos vs. NKG2A-neg expressing NK cells and to generate the NKG2A+pos/NKG2A-neg ratio in the bone marrow blood collected three months after the AuSCT.
Results: With a median follow-up of 36 months, we found that the NKG2A+pos/NKG2A-neg ratio no higher than 0.4 (<=0.4), a cut-off chosen from our normal healthy donors (n=4), was a prognostic factor associated with significantly longer RP than those who had the ratio > 0.4 (mean [95% CI], not reached [42.4-54.6] vs. 24 months [22.9-40.7]; p=.006, respectively). Multivariate analysis showed that the ratio <= 0.4 was an independent factor from the other conventional prognostic factors for RP. Furthermore, differential expression analysis regarding subgroups of these NK cells showed more 2DL-3DL-2DS- and 2DL3+3DL-2DS- cell groups in the patient population with the ratio <=0.4 (p <.001 and 0.021, respectively).
Conclusions: In conclusion, this is the first study to show NKG2A+pos/NKG2A-neg ratio could be a novel immunomicroenvironment related factor to predict RP for MM patients who have received AuSCT and which also highlight a translational potential by targeting NKG2A as a post AuSCT maintenance strategy.
Methods: During May 2019 and Jun 2022, we prospectively enrolled 69 MM patients who had received nearly uniform induction followed by AuSCT and thalidomide maintenance. By using flow cytometry, we evaluated the percent of NKG2A+pos vs. NKG2A-neg expressing NK cells and to generate the NKG2A+pos/NKG2A-neg ratio in the bone marrow blood collected three months after the AuSCT.
Results: With a median follow-up of 36 months, we found that the NKG2A+pos/NKG2A-neg ratio no higher than 0.4 (<=0.4), a cut-off chosen from our normal healthy donors (n=4), was a prognostic factor associated with significantly longer RP than those who had the ratio > 0.4 (mean [95% CI], not reached [42.4-54.6] vs. 24 months [22.9-40.7]; p=.006, respectively). Multivariate analysis showed that the ratio <= 0.4 was an independent factor from the other conventional prognostic factors for RP. Furthermore, differential expression analysis regarding subgroups of these NK cells showed more 2DL-3DL-2DS- and 2DL3+3DL-2DS- cell groups in the patient population with the ratio <=0.4 (p <.001 and 0.021, respectively).
Conclusions: In conclusion, this is the first study to show NKG2A+pos/NKG2A-neg ratio could be a novel immunomicroenvironment related factor to predict RP for MM patients who have received AuSCT and which also highlight a translational potential by targeting NKG2A as a post AuSCT maintenance strategy.
