Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-322: Real world outcomes of belantamab mafodotin from the UK and Ireland: updated results.
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST

Edmund Watson, MD
PhD Student; Haematology Registrar
University of Oxford
Oxford, United Kingdom
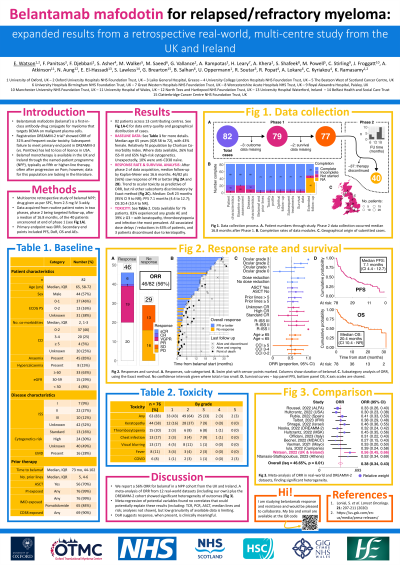
Introduction: Belantamab mafodotin (belamaf) is an antibody-drug conjugate therapy for myeloma that targets BCMA on malignant plasma cells. Its role in relapsed/refractory myeloma was demonstrated in the DREAMM-2 trial, where it associated with an overall response rate (ORR) of 31% and frequent ocular toxicity – outcomes that have been replicated in retrospective studies across Europe and the USA. Belamaf monotherapy is available in the UK and Ireland through the named-patient programme (NPP), typically as fifth or higher-line therapy and often after disease progression on pomalidomide; however, outcome data for this population are lacking in the literature.
Methods: We conducted a multicentre retrospective study across the UK and Ireland of patients receiving belamaf monotherapy within the NPP. Belamaf was administered as per the summary of product characteristics, starting at 2.5 mg intravenously every three weeks. Contributors entered data from routine patient notes into a secure online form. Case registration ran from January 2022 to June 2022 (extending to March 2023 for one centre). Data were cleaned in Microsoft Excel and the Tidyverse for R. Analysis was performed on Stata. The primary endpoint was ORR. Secondary end points included progression-free survival (PFS), duration of response (DOR), overall survival (OS) and adverse events (AEs). The Kaplan-Meier method was used for survival analysis.
Results: 81 patients were registered across thirteen contributing centres. The median age was 65 years (IQR 58 to 72), with 43% female. Median Charlson co-morbidity index was 2. Where data were available, 26% patients had ISS-III and 65% high-risk cytogenetics. Median lines prior therapy was 5 (IQR 4 to 6), with median time from diagnosis to belamaf of 73 months. 70% patients had had prior autologous stem cell transplant. Unexpectedly, 10% were anti-CD38 naïve.
At an interim analysis, with median follow-up of 6.6 months and 4 cycles administered (IQR 2 to 6), 48% (n = 39) had discontinued therapy (PD 40%, death 6%, toxicity 1%, unknown 1%). ORR was 56% with at least VGPR in 30%. Median PFS was 9.3 months (95% CI 3.7 to 13.1); median DOR was 15.9 months (4.1 to not reached); and median OS 17.8 months (7.6 to not reached). Data collection for extended survival analysis is ongoing.
Toxicity data were available for 76 patients. 83% experienced any grade AE, the most common being keratopathy, infection and thrombocytopenia, affecting 58%, 36% and 20% of patients, respectively. These were also the most frequent ≥ grade 3 AEs; infection affected 30% of patients (with 4% COVID-related deaths), thrombocytopenia 11%, and keratopathy 7%. AE-associated dose delays or reductions occurred in 43% of patients.
Conclusions: We report an ORR of 56% in our cohort of UK and Ireland patients receiving belamaf monotherapy under the NPP. We will present at the meeting extended follow-up results and an analysis across clinically relevant covariates to compare these outcomes with other studies of belamaf monotherapy.
Methods: We conducted a multicentre retrospective study across the UK and Ireland of patients receiving belamaf monotherapy within the NPP. Belamaf was administered as per the summary of product characteristics, starting at 2.5 mg intravenously every three weeks. Contributors entered data from routine patient notes into a secure online form. Case registration ran from January 2022 to June 2022 (extending to March 2023 for one centre). Data were cleaned in Microsoft Excel and the Tidyverse for R. Analysis was performed on Stata. The primary endpoint was ORR. Secondary end points included progression-free survival (PFS), duration of response (DOR), overall survival (OS) and adverse events (AEs). The Kaplan-Meier method was used for survival analysis.
Results: 81 patients were registered across thirteen contributing centres. The median age was 65 years (IQR 58 to 72), with 43% female. Median Charlson co-morbidity index was 2. Where data were available, 26% patients had ISS-III and 65% high-risk cytogenetics. Median lines prior therapy was 5 (IQR 4 to 6), with median time from diagnosis to belamaf of 73 months. 70% patients had had prior autologous stem cell transplant. Unexpectedly, 10% were anti-CD38 naïve.
At an interim analysis, with median follow-up of 6.6 months and 4 cycles administered (IQR 2 to 6), 48% (n = 39) had discontinued therapy (PD 40%, death 6%, toxicity 1%, unknown 1%). ORR was 56% with at least VGPR in 30%. Median PFS was 9.3 months (95% CI 3.7 to 13.1); median DOR was 15.9 months (4.1 to not reached); and median OS 17.8 months (7.6 to not reached). Data collection for extended survival analysis is ongoing.
Toxicity data were available for 76 patients. 83% experienced any grade AE, the most common being keratopathy, infection and thrombocytopenia, affecting 58%, 36% and 20% of patients, respectively. These were also the most frequent ≥ grade 3 AEs; infection affected 30% of patients (with 4% COVID-related deaths), thrombocytopenia 11%, and keratopathy 7%. AE-associated dose delays or reductions occurred in 43% of patients.
Conclusions: We report an ORR of 56% in our cohort of UK and Ireland patients receiving belamaf monotherapy under the NPP. We will present at the meeting extended follow-up results and an analysis across clinically relevant covariates to compare these outcomes with other studies of belamaf monotherapy.
