Treatment of Newly Diagnosed Myeloma - Non-Transplant Eligible
Poster Session 1
P-121: Real World Outcomes of Undocumented Multiple Myeloma Patients: A Safety Net Hospital Experience
Wednesday, September 27, 2023
1:30 PM - 2:30 PM EEST

Aishwarya Sannareddy, MBBS (she/her/hers)
Senior Researcher
UT Southwestern Medical Center
Dallas, Texas, United States
Introduction: There are approximately 16-29 million undocumented immigrants (UI) in United States (US). UIs face more 2-fold problems in seeking medical care compared to the general population due to various financial and social burdens which include fear of deportation, language barriers, and low socioeconomic status. Most UIs are not eligible for Medicaid, state-based or employer-sponsored coverage plans, and rely on safety net hospital systems. UIs diagnosed with hematological malignancies, such as multiple myeloma (MM), face additional burdens of financially prohibitive therapies and the need for frequent provider and infusion visits. Studies have shown that immigration status can lead to disparate health outcomes, but these outcomes are poorly defined. In this study, we aim to highlight the real-world outcomes of a unique population of UIs diagnosed with MM.
Methods: We performed a retrospective analysis on 450 patients (pts) treated for MM at Parkland Health from 1997 to 2022. Pts were considered undocumented if a valid social security number was unavailable in their electronic health record or did not qualify for a state-based insurance plan. All pts were “transplant-ineligible” due to financial constraints and lack of insurance coverage. Most pts were able to access reduced cost MM therapies through Parkland's financial assistance program. We performed a survival analysis to assess the overall survival outcomes.
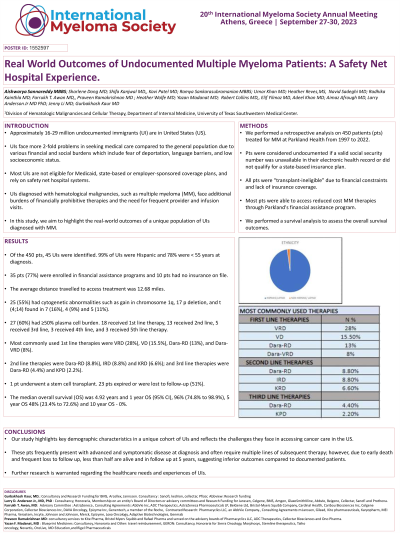
Results: Of the 450 pts, 45 UIs were identified. 99% of UIs were Hispanic and 78% were < 55 years at diagnosis. 35 pts (77%) were enrolled in financial assistance programs and 10 pts had no insurance on file. The average distance travelled to access treatment was 12.68 miles. 25 (55%) had cytogenetic abnormalities such as gain in chromosome 1q, 17 p deletion, and t (4;14) found in 7 (16%), 4 (9%) and 5 (11%). 27 (60%) had ≥50% plasma cell burden. 18 received 1st line therapy, 13 received 2nd line, 5 received 3rd line, 3 received 4th line, and 3 received 5th line therapy. Most commonly used 1st line therapies were VRD (28%), VD (15.5%), Dara-RD (13%), and Dara-VRD (8%). 2nd line therapies were Dara-RD (8.8%), IRD (8.8%) and KRD (6.6%); and 3rd line therapies were Dara-RD (4.4%) and KPD (2.2%). 1 pt underwent a stem cell transplant. 23 pts expired or were lost to follow-up (51%). The median overall survival (OS) was 4.92 years and 1 year OS (95% CI), 96% (74.8% to 98.9%), 5 year OS 48% (23.4% to 72.6%) and 10 year OS - 0%.
Conclusions: Our study highlights key demographic characteristics in a unique cohort of UIs and reflects the challenges they face in accessing cancer care in the US. These pts frequently present with advanced and symptomatic disease at diagnosis and often require multiple lines of subsequent therapy; however, due to early death and frequent loss to follow up, less than half are alive and in follow up at 5 years, suggesting inferior outcomes compared to documented patients. Further research is warranted regarding the healthcare needs and experiences of UIs.
Methods: We performed a retrospective analysis on 450 patients (pts) treated for MM at Parkland Health from 1997 to 2022. Pts were considered undocumented if a valid social security number was unavailable in their electronic health record or did not qualify for a state-based insurance plan. All pts were “transplant-ineligible” due to financial constraints and lack of insurance coverage. Most pts were able to access reduced cost MM therapies through Parkland's financial assistance program. We performed a survival analysis to assess the overall survival outcomes.
Results: Of the 450 pts, 45 UIs were identified. 99% of UIs were Hispanic and 78% were < 55 years at diagnosis. 35 pts (77%) were enrolled in financial assistance programs and 10 pts had no insurance on file. The average distance travelled to access treatment was 12.68 miles. 25 (55%) had cytogenetic abnormalities such as gain in chromosome 1q, 17 p deletion, and t (4;14) found in 7 (16%), 4 (9%) and 5 (11%). 27 (60%) had ≥50% plasma cell burden. 18 received 1st line therapy, 13 received 2nd line, 5 received 3rd line, 3 received 4th line, and 3 received 5th line therapy. Most commonly used 1st line therapies were VRD (28%), VD (15.5%), Dara-RD (13%), and Dara-VRD (8%). 2nd line therapies were Dara-RD (8.8%), IRD (8.8%) and KRD (6.6%); and 3rd line therapies were Dara-RD (4.4%) and KPD (2.2%). 1 pt underwent a stem cell transplant. 23 pts expired or were lost to follow-up (51%). The median overall survival (OS) was 4.92 years and 1 year OS (95% CI), 96% (74.8% to 98.9%), 5 year OS 48% (23.4% to 72.6%) and 10 year OS - 0%.
Conclusions: Our study highlights key demographic characteristics in a unique cohort of UIs and reflects the challenges they face in accessing cancer care in the US. These pts frequently present with advanced and symptomatic disease at diagnosis and often require multiple lines of subsequent therapy; however, due to early death and frequent loss to follow up, less than half are alive and in follow up at 5 years, suggesting inferior outcomes compared to documented patients. Further research is warranted regarding the healthcare needs and experiences of UIs.
