Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-246: Real-world attrition rates after second-line therapy or later in patients from the Flatiron database with relapsed/refractory multiple myeloma refractory to lenalidomide
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST
Binod Dhakal, MD, MS
Associate Professor
Medical College of Wisconsin, Milwaukee, WI, USA, United States
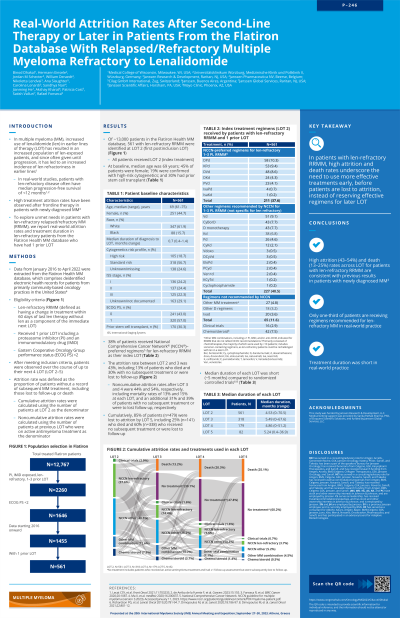
Introduction: To explore unmet need in patients with relapsed/refractory multiple myeloma (RRMM) refractory to lenalidomide (len), we report real-world attrition rates and treatment duration for len-refractory patients from the Flatiron multiple myeloma (MM) database who have had 1 prior line of therapy (LOT).
Methods: Data from January 2016 to April 2022 were extracted from the Flatiron Health deidentified US electronic health records database. Eligible patients had len-refractory RRMM (defined as having a change in treatment within 60 days of last len therapy without len as a component of the immediate next LOT), 1 prior LOT including a proteasome inhibitor and an immunomodulatory drug, and an ECOG performance status < 2. After meeting inclusion criteria, patients were observed over their next 4 LOTs (LOT 2–5). Attrition rate was defined as the proportion of patients without a record of subsequent MM treatment.
Results: From ~13,000 patients in the Flatiron database, we identified 561 at LOT 2 (first postinclusion LOT) with len-refractory RRMM. All patients received LOT 2. The attrition rate between LOT 2 and 3 was 43%, including 13% of patients who died and 30% with no subsequent treatment or lost follow-up. Noncumulative attrition rates after LOT 3 and 4 were 44% and 54%, respectively, including mortality rates of 13% and 15% at each LOT and an additional 31% and 39% of patients with no subsequent treatment or lost follow-up. Cumulatively, 85% patients (n=479) were lost to attrition by LOT 5, including 25% patients (n=141) who died and 60% patients (n=338) who received no subsequent treatment or were lost to follow-up. In LOT 2, 3, 4, and 5, a respective 38%, 14%, 8%, and 4% of the 561 patients received a National Comprehensive Cancer Network (NCCN)-recommended regimen (NCCN Guidelines for MM, Version 3. 2023) for len-refractory RRMM; and 41%, 26%, 14%, and 5% received other NCCN-endorsed RRMM regimens. In each of LOTs 2–5, 0.7–2.9% of the 561 patients participated in clinical trials. Median duration of each LOT was 4.5 month in LOT 2, 5.5 month in LOT 3, 4.9 month in LOT 4, and 5.2 month in LOT 5.
Conclusions: Our findings of high attrition rates across LOTs (43–54%) for patients with len-refractory RRMM are consistent with previous results in patients with newly diagnosed MM (eligible and ineligible for transplant). In published literature, attrition rates were 21–57% after LOT 1 and 31–46% for the next 3 LOTs. The short median durations of treatment (each LOT < 6 month) observed in this analysis highlights the ineffectiveness of existing therapies. Together, these data underscore the need for more effective treatments early, before patients are lost to attrition, instead of reserving effective regimens for later LOTs.
Methods: Data from January 2016 to April 2022 were extracted from the Flatiron Health deidentified US electronic health records database. Eligible patients had len-refractory RRMM (defined as having a change in treatment within 60 days of last len therapy without len as a component of the immediate next LOT), 1 prior LOT including a proteasome inhibitor and an immunomodulatory drug, and an ECOG performance status < 2. After meeting inclusion criteria, patients were observed over their next 4 LOTs (LOT 2–5). Attrition rate was defined as the proportion of patients without a record of subsequent MM treatment.
Results: From ~13,000 patients in the Flatiron database, we identified 561 at LOT 2 (first postinclusion LOT) with len-refractory RRMM. All patients received LOT 2. The attrition rate between LOT 2 and 3 was 43%, including 13% of patients who died and 30% with no subsequent treatment or lost follow-up. Noncumulative attrition rates after LOT 3 and 4 were 44% and 54%, respectively, including mortality rates of 13% and 15% at each LOT and an additional 31% and 39% of patients with no subsequent treatment or lost follow-up. Cumulatively, 85% patients (n=479) were lost to attrition by LOT 5, including 25% patients (n=141) who died and 60% patients (n=338) who received no subsequent treatment or were lost to follow-up. In LOT 2, 3, 4, and 5, a respective 38%, 14%, 8%, and 4% of the 561 patients received a National Comprehensive Cancer Network (NCCN)-recommended regimen (NCCN Guidelines for MM, Version 3. 2023) for len-refractory RRMM; and 41%, 26%, 14%, and 5% received other NCCN-endorsed RRMM regimens. In each of LOTs 2–5, 0.7–2.9% of the 561 patients participated in clinical trials. Median duration of each LOT was 4.5 month in LOT 2, 5.5 month in LOT 3, 4.9 month in LOT 4, and 5.2 month in LOT 5.
Conclusions: Our findings of high attrition rates across LOTs (43–54%) for patients with len-refractory RRMM are consistent with previous results in patients with newly diagnosed MM (eligible and ineligible for transplant). In published literature, attrition rates were 21–57% after LOT 1 and 31–46% for the next 3 LOTs. The short median durations of treatment (each LOT < 6 month) observed in this analysis highlights the ineffectiveness of existing therapies. Together, these data underscore the need for more effective treatments early, before patients are lost to attrition, instead of reserving effective regimens for later LOTs.
