Other plasma cell disorders
Poster Session 3
P-429: Real-world data of zanubrutinib treatment for patients with previously treated Waldenstrom Macroglobulinemia
Friday, September 29, 2023
1:15 PM - 2:15 PM EEST

Seo Yoon Jang
Resident
Department of Internal Medicine, Seoul National University Hospital, Seoul, South Korea, Republic of Korea
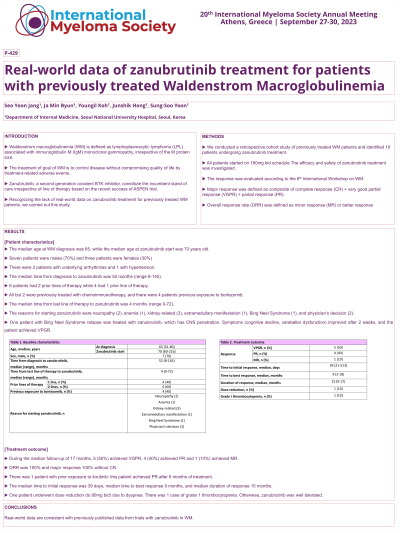
Introduction: Waldenstrom macroglobulinemia (WM) is defined as lymphoplasmacytic lymphoma (LPL) associated with immunoglobulin M (IgM) monoclonal gammopathy, irrespective of the M protein size. The treatment of goal of WM is to control disease without compromising quality of life by treatment-related adverse events. Zanubrutinib, a second generation covalent BTK inhibitor, constitute the incumbent stand of care irrespective of line of therapy based on the recent success of ASPEN trial. Recognizing the lack of real-world data on zanubrutinib treatment for previously treated WM patients, we carried out this study.
Methods: We conducted a retrospective cohort study of previously treated WM patients and identified 10 patients undergoing zanubrutinib treatment. All patients started on 160mg bid schedule The efficacy and safety of zanubrutinib treatment was investigated. The response was evaluated according to the 6th International Workshop on WM. Major response was defined as composite of complete response (CR) + very good partial response (VGPR) + partial response (PR). Overall response rate (ORR) was defined as minor response (MR) or better response.
Results: The median age at WM diagnosis was 65, while the median age at zanubrutinib start was 70 years old. There were 7 males and 3 females. There were 2 patients with underlying arrhythmias and 1 with hypertension. The median time from diagnosis to zanubrutinib was 52 months (range 8-145), and 6 patients had 2 prior lines of therapy while 4 had 1 prior line of therapy. All but 2 were previously treated with chemoimmunotherapy, and there were 4 patients previous exposure to bortezomib. The median time from last line of therapy to zanubrutinib was 4 months (range 0-72 months). The reason for starting zanubrutinib were neuropathy (2), anemia (1), kidney-related (3), extramedullary manifestation (1), Bing Neel Syndrome (1), and physician’s decision (2). During the median follow-up of 17 months, 5 (50%) achieved VGPR, 4 (40%) achieved PR and 1 (10%) achieved MR. ORR was 100% and major response 100% without CR. There was 1 patient with prior exposure to ibrutinib: this patient achieved PR after 6 months of treatment. The median time to initial response was 39 days, median time to best response 9 months, and median duration of response 15 months.
One patient underwent dose reduction (to 80mg bid) due to dyspnea. There was 1 case of grade 1 thrombocytopenia. Otherwise, zanubrutinib was well tolerated.
Conclusions: Real-world data are consistent with previously published data from trials with zanubrutinib in WM.
Methods: We conducted a retrospective cohort study of previously treated WM patients and identified 10 patients undergoing zanubrutinib treatment. All patients started on 160mg bid schedule The efficacy and safety of zanubrutinib treatment was investigated. The response was evaluated according to the 6th International Workshop on WM. Major response was defined as composite of complete response (CR) + very good partial response (VGPR) + partial response (PR). Overall response rate (ORR) was defined as minor response (MR) or better response.
Results: The median age at WM diagnosis was 65, while the median age at zanubrutinib start was 70 years old. There were 7 males and 3 females. There were 2 patients with underlying arrhythmias and 1 with hypertension. The median time from diagnosis to zanubrutinib was 52 months (range 8-145), and 6 patients had 2 prior lines of therapy while 4 had 1 prior line of therapy. All but 2 were previously treated with chemoimmunotherapy, and there were 4 patients previous exposure to bortezomib. The median time from last line of therapy to zanubrutinib was 4 months (range 0-72 months). The reason for starting zanubrutinib were neuropathy (2), anemia (1), kidney-related (3), extramedullary manifestation (1), Bing Neel Syndrome (1), and physician’s decision (2). During the median follow-up of 17 months, 5 (50%) achieved VGPR, 4 (40%) achieved PR and 1 (10%) achieved MR. ORR was 100% and major response 100% without CR. There was 1 patient with prior exposure to ibrutinib: this patient achieved PR after 6 months of treatment. The median time to initial response was 39 days, median time to best response 9 months, and median duration of response 15 months.
One patient underwent dose reduction (to 80mg bid) due to dyspnea. There was 1 case of grade 1 thrombocytopenia. Otherwise, zanubrutinib was well tolerated.
Conclusions: Real-world data are consistent with previously published data from trials with zanubrutinib in WM.
