Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-321: Real-World Outcomes In Myeloma Patients With t(11;14): A Matched Comparison Using the Canadian Myeloma Research Group National Clinical Database
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST

Julia Varghese, MD, FRCPC
Fellow
British Columbia Cancer Agency and University of British Columbia
Vancouver, British Columbia, Canada
Introduction: In myeloma, t(11;14) confers a unique biology including a lymphoplasmacytic phenotype and an association with plasma cell leukemia. Some studies report a favourable while others a worse prognosis, compared to non-t(11;14) cases. Dependence of t(11;14) cells on the BCL-2 pathway offers a potential therapeutic target. We performed a matched comparison of real-world outcomes in patients with and without t(11;14) as a benchmark for future therapy targeting BCL-2
Methods: Using the Canadian Myeloma Research Group Database, we identified patients with a t(11;14) diagnosed from 2004-22. Patients were matched with a non-t(11;14) cohort based on age at line 1 of therapy, gender, year of diagnosis and history of ASCT. Outcomes were examined over the first 4 therapy lines. Differences in baseline characteristics, response, and drug exposure were assessed by McNemar’s test and Wilcoxon Signed Rank test. Progression-free (PFS) and overall survival (OS) were calculated by the Kaplan-Meier product-limit method
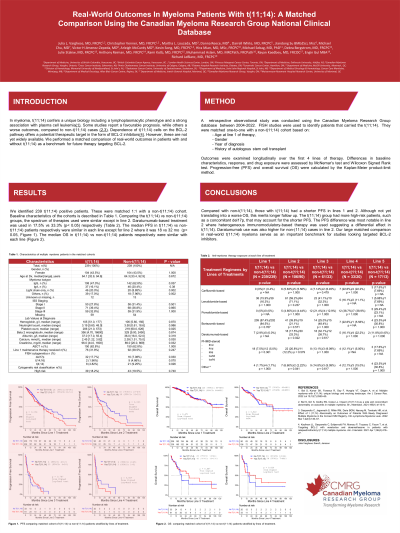
Results: 234 t(11;14) patients were matched 1:1 with a non-t(11;14) cohort. Baseline characteristics were similar aside from more patients with light chain myeloma (20.0% vs 8.85%; p < 0.05), hyposecretory/oligosecretory/non-IgA/G subtypes (17.0% vs 7.96%; p< 0.05), and del17p (17.7% vs 7.08%; p< 0.05) in the t(11;14) cohort. Comparing the t(11;14) vs non-t(11;14) groups, the majority of patients received bortezomib-based treatment in line 1 (87.4% vs 84.5%; p=0.767) and 62.8% in each arm underwent ASCT. The most common regimens in line 2 were lenalidomide-based (59.2% vs 77.0%; p=0.24) followed by bortezomib-based treatment (39.8% vs 21.1%; p=0.57). In line 2, daratumumab-based treatment was used in 20.3% vs 30.9% (p < 0.05) respectively. Further regimen details will be presented at the meeting. The median PFS in t(11;14) vs non-t(11;14) patients respectively were 44 vs 46 mo (p < 0.05) after line 1, 18 vs 32 mo (p < 0.05) for line 2, 6 vs 13 mo (p=0.79) for line 3 and 3 vs 6 mo (p=0.83) for line 4 treatment. The median OS in t(11;14) vs non-t(11;14) patients respectively were 99 mo vs 128 mo (p=0.47) after line 1, 77 mo in each cohort (p=0.82) after line 2, 43 vs 26 mo (p=0.44) after line 3 and 34 vs 15 mo after line 4 (p=0.82)
Conclusions: Compared with non-t(11;14), those with t(11;14) had a shorter PFS in lines 1 and 2. Although not yet translating into a worse OS, this merits longer follow up. The t(11;14) group had more high-risk patients that may account for the shorter PFS. A higher-risk molecular subset with concurrent mutated CCND1 may also be present. The PFS difference was most notable in line 2 where heterogenous immunomodulatory-based therapy was used suggesting a differential effect in t(11;14). Daratumumab use was also higher for non-(11;14) cases in line 2. Our large matched comparison in real-world t(11;14) myeloma serves as an important benchmark for studies looking at targeted BCL-2 inhibitors in these patients
Methods: Using the Canadian Myeloma Research Group Database, we identified patients with a t(11;14) diagnosed from 2004-22. Patients were matched with a non-t(11;14) cohort based on age at line 1 of therapy, gender, year of diagnosis and history of ASCT. Outcomes were examined over the first 4 therapy lines. Differences in baseline characteristics, response, and drug exposure were assessed by McNemar’s test and Wilcoxon Signed Rank test. Progression-free (PFS) and overall survival (OS) were calculated by the Kaplan-Meier product-limit method
Results: 234 t(11;14) patients were matched 1:1 with a non-t(11;14) cohort. Baseline characteristics were similar aside from more patients with light chain myeloma (20.0% vs 8.85%; p < 0.05), hyposecretory/oligosecretory/non-IgA/G subtypes (17.0% vs 7.96%; p< 0.05), and del17p (17.7% vs 7.08%; p< 0.05) in the t(11;14) cohort. Comparing the t(11;14) vs non-t(11;14) groups, the majority of patients received bortezomib-based treatment in line 1 (87.4% vs 84.5%; p=0.767) and 62.8% in each arm underwent ASCT. The most common regimens in line 2 were lenalidomide-based (59.2% vs 77.0%; p=0.24) followed by bortezomib-based treatment (39.8% vs 21.1%; p=0.57). In line 2, daratumumab-based treatment was used in 20.3% vs 30.9% (p < 0.05) respectively. Further regimen details will be presented at the meeting. The median PFS in t(11;14) vs non-t(11;14) patients respectively were 44 vs 46 mo (p < 0.05) after line 1, 18 vs 32 mo (p < 0.05) for line 2, 6 vs 13 mo (p=0.79) for line 3 and 3 vs 6 mo (p=0.83) for line 4 treatment. The median OS in t(11;14) vs non-t(11;14) patients respectively were 99 mo vs 128 mo (p=0.47) after line 1, 77 mo in each cohort (p=0.82) after line 2, 43 vs 26 mo (p=0.44) after line 3 and 34 vs 15 mo after line 4 (p=0.82)
Conclusions: Compared with non-t(11;14), those with t(11;14) had a shorter PFS in lines 1 and 2. Although not yet translating into a worse OS, this merits longer follow up. The t(11;14) group had more high-risk patients that may account for the shorter PFS. A higher-risk molecular subset with concurrent mutated CCND1 may also be present. The PFS difference was most notable in line 2 where heterogenous immunomodulatory-based therapy was used suggesting a differential effect in t(11;14). Daratumumab use was also higher for non-(11;14) cases in line 2. Our large matched comparison in real-world t(11;14) myeloma serves as an important benchmark for studies looking at targeted BCL-2 inhibitors in these patients
