Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-248: REAL-WORLD OUTCOMES OF TRIPLE-CLASS EXPOSED MULTIPLE MYELOMA PATIENTS BY TREATMENT EXPERIENCE: THE ASSOCIATION OF PRIOR LINES AND PENTA-REFRACTORINESS WITH PROGRESSION-FREE AND OVERALL SURVIVAL
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST

Marco DiBonaventura, PhD (he/him/his)
Senior Director, Value & Evidence Team Lead, Hematology & Biosimilars
Pfizer Inc
New York, New York, United States
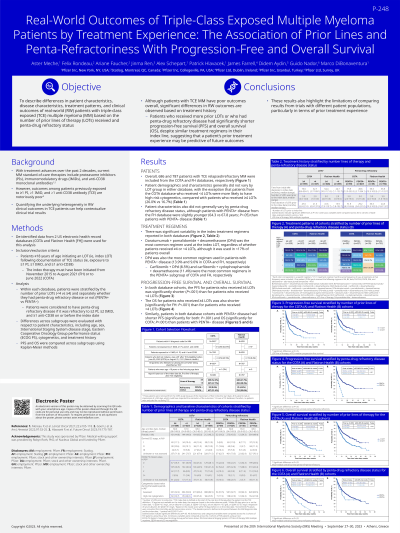
Introduction: Outcomes among patients (pts) with multiple myeloma (MM) who have been exposed to at least 1 proteasome inhibitor (PI), 1 immunomodulatory (IMiD) drug, and 1 anti-CD38 antibody (triple-class exposed [TCE]) are notoriously poor. The current study sought to quantify the underlying heterogeneity in clinical outcomes by stratifying TCE pts by their treatment experience using real-world data sources.
Methods: TCE MM pts ≥18 years who had initiated a subsequent therapy (ie, index regimen) after this point were identified from two US electronic health record databases: COTA and Flatiron Health (FH). Within each database, pts were stratified by the number of lines of therapy (LOT) that they had been exposed to ( < 4 vs ≥4, based on the distribution) and, separately, whether they were penta-refractory (yes [PENTA+] vs no [PENTA-]). Differences across subgroups were evaluated with respect to patient (pt) characteristics (age, sex, ISS, ECOG, cytogenetics) and treatment history. Progression-free survival (PFS) and overall survival (OS) were compared across these subgroups using Kaplan-Meier methods.
Results: N=686 TCE MM pts were included from the COTA database (52.3% had received ≥4 LOT [range 4-14]; 8.6% were PENTA+). Pts with fewer LOT were more likely to have high-risk cytogenetics (26.0% vs 16.7%) but the pt characteristics were otherwise generally similar to pts with ≥4 LOT. There was significant variability in the index treatment regimen, but daratumumab+pomalidomide+ dexamethasone (DPd) (13.5% and 9.7%, respectively) was the most common index regimen for both subgroups. No pt characteristic varied by PENTA status, though DPd was more common among those who were PENTA- (12.0% vs 6.8%). N=787 TCE MM pts were included from the FH database (41.7% had received ≥4 LOT; 4.4% were PENTA+). Pt characteristics did not vary by LOT group; DPd was the most common regimen for both < 4 LOT (7.3%) and ≥4 LOT (9.8%). PENTA+ pts were slightly younger (64.3 vs 67.8 yrs, p<.05) but otherwise similar to PENTA- pts. DPd (9.0%) was the most common regimen among PENTA- while carfilzomib+cyclophosphamide+dexamethasone (11.4%) was the most common regimen among PENTA+ pts. Pts with ≥4 LOT reported shorter PFS than pts with < 4 LOT (medians: 6.1 vs 17.8 months [COTA]; 7.3 vs 16.6 months [FH]; log-rank ps <.05) and OS (medians: 19.4 vs 24.5 months [COTA], log-rank p=.10; 14.2 vs 33.0 months [FH], log-rank p<.05). Similarly, pts who were PENTA+ had shorter PFS than PENTA- (medians: 4.7 vs 10.2 months [COTA]; 3.7 vs 14.8 months [FH]; log-rank ps <.05) and OS (medians: 14.3 vs 21.9 months [COTA], log-rank p<.05; 11.8 vs 21.3 months [FH], log-rank p=.21).
Conclusions: Although TCE MM pts report poor outcomes overall, significant differences in real-world outcomes are observed based on their treatment histories. Pts with more prior LOTs or who were penta-refractory had significantly shorter PFS and OS, despite similar treatment regimens in their index line.
Methods: TCE MM pts ≥18 years who had initiated a subsequent therapy (ie, index regimen) after this point were identified from two US electronic health record databases: COTA and Flatiron Health (FH). Within each database, pts were stratified by the number of lines of therapy (LOT) that they had been exposed to ( < 4 vs ≥4, based on the distribution) and, separately, whether they were penta-refractory (yes [PENTA+] vs no [PENTA-]). Differences across subgroups were evaluated with respect to patient (pt) characteristics (age, sex, ISS, ECOG, cytogenetics) and treatment history. Progression-free survival (PFS) and overall survival (OS) were compared across these subgroups using Kaplan-Meier methods.
Results: N=686 TCE MM pts were included from the COTA database (52.3% had received ≥4 LOT [range 4-14]; 8.6% were PENTA+). Pts with fewer LOT were more likely to have high-risk cytogenetics (26.0% vs 16.7%) but the pt characteristics were otherwise generally similar to pts with ≥4 LOT. There was significant variability in the index treatment regimen, but daratumumab+pomalidomide+ dexamethasone (DPd) (13.5% and 9.7%, respectively) was the most common index regimen for both subgroups. No pt characteristic varied by PENTA status, though DPd was more common among those who were PENTA- (12.0% vs 6.8%). N=787 TCE MM pts were included from the FH database (41.7% had received ≥4 LOT; 4.4% were PENTA+). Pt characteristics did not vary by LOT group; DPd was the most common regimen for both < 4 LOT (7.3%) and ≥4 LOT (9.8%). PENTA+ pts were slightly younger (64.3 vs 67.8 yrs, p<.05) but otherwise similar to PENTA- pts. DPd (9.0%) was the most common regimen among PENTA- while carfilzomib+cyclophosphamide+dexamethasone (11.4%) was the most common regimen among PENTA+ pts. Pts with ≥4 LOT reported shorter PFS than pts with < 4 LOT (medians: 6.1 vs 17.8 months [COTA]; 7.3 vs 16.6 months [FH]; log-rank ps <.05) and OS (medians: 19.4 vs 24.5 months [COTA], log-rank p=.10; 14.2 vs 33.0 months [FH], log-rank p<.05). Similarly, pts who were PENTA+ had shorter PFS than PENTA- (medians: 4.7 vs 10.2 months [COTA]; 3.7 vs 14.8 months [FH]; log-rank ps <.05) and OS (medians: 14.3 vs 21.9 months [COTA], log-rank p<.05; 11.8 vs 21.3 months [FH], log-rank p=.21).
Conclusions: Although TCE MM pts report poor outcomes overall, significant differences in real-world outcomes are observed based on their treatment histories. Pts with more prior LOTs or who were penta-refractory had significantly shorter PFS and OS, despite similar treatment regimens in their index line.
