Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-257: Real-world treatment patterns and clinical outcomes among patients with triple-class exposed (TCE) multiple myeloma (MM)
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST

Rafael Fonseca, MD
Chief Innovation Officer
Division of Hematology/Oncology, Mayo Clinic, Phoenix, AZ, USA
Phoenix, Arizona, United States
Introduction: Despite the advancements in available therapeutics for MM, MM remains an incurable disease, and most patients relapse and require further treatment. Patients who are TCE to immunomodulatory drugs, proteasome inhibitors, and anti-CD38 monoclonal antibodies have particularly high unmet needs. With rapid treatment landscape changes, the aim of this study is to describe characteristics, treatment patterns, and clinical outcomes of these patients in recent years.
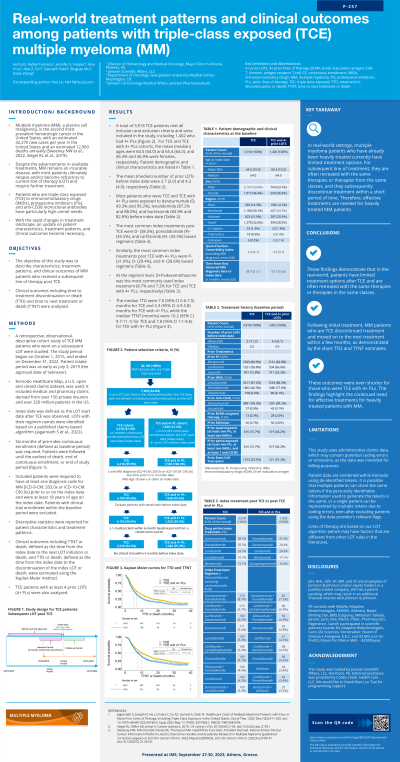
Methods: Patients with MM who started subsequent line of treatment (LOT) after they were TCE from July 03, 2019 (Selinexor approval date) to December 31, 2020 were selected from the Komodo Healthcare Map—a US claims dataset and were followed until the earliest of death, last claim, or end of study period (June 30, 2021). The primary analysis included patients with a subsequent LOT after becoming TCE. Patients who were post TCE with 4+ PLs and quadruple-class exposed (QCE; TCE + exposed to B-cell maturation antigen targeted drug) were also analyzed. Index date was defined as LOT start date after each exposure definitions. Descriptive statistics were reported for patient characteristics and treatment patterns. Clinical outcomes such as time to treatment discontinuation or death (TTD), and time to next treatment or death (TTNT) were estimated using the Kaplan-Meier method. Here we reported data for TCE and TCE with 4+ prior PLs; data for QCE cohort will be presented in the future.
Results: A total of 1,704 TCE patients were included, among whom 1,072 had 4+ PLs. For TCE and TCE with 4+ PLs cohorts, the mean (median) ages were 64.6 (64.0) and 64.9 (64.0), and 46.6% and 47.4% were females, respectively. The mean (median) number of prior LOTs before index date were 3.9 (4.0) and 4.7 (4.0), respectively. Most patients who were TCE and TCE with 4+ PLs were exposed to daratumumab (D; 99.9% and 99.8%), lenalidomide (85.6% and 86.4 %), and bortezomib (84.2 % and 83.0%) before index date. The most common post-TCE treatments were pomalidomide (P)- (36.0%), D- (35.0%), and carfilzomib (K)- (33.7%) based regimens. Similarly, the most common post-TCE with 4+ PLs treatments were P- (33.8%), K- (33.8%), and D- (30.5%) based regimens. At the regimen level, D+P±dexamethasone was the most commonly used post-index regimen (8.0% and 6.7% for TCE and TCE with 4+ PLs, respectively). The median TTD (months) were 5.8 (95% CI 5.4-6.5) for TCE and 5.1 (95% CI 4.8-5.6) for TCE with 4+ PLs, while the median TTNT (months) were 8.4 (95% CI 7.9-9.4) for TCE and 7.1 (95% CI 6.7-7.8) for TCE with 4+ PLs.
Conclusions: These findings demonstrate that in the real-world, patients have limited treatment options after TCE and are often retreated with the same therapies or therapies in the same classes. Patients who were TCE discontinued treatment and moved on to next treatment shortly after initial treatment. These outcomes were even shorter for those with 4+ PLs. The findings highlight the continued need for effective treatments for heavily treated patients with MM.
Methods: Patients with MM who started subsequent line of treatment (LOT) after they were TCE from July 03, 2019 (Selinexor approval date) to December 31, 2020 were selected from the Komodo Healthcare Map—a US claims dataset and were followed until the earliest of death, last claim, or end of study period (June 30, 2021). The primary analysis included patients with a subsequent LOT after becoming TCE. Patients who were post TCE with 4+ PLs and quadruple-class exposed (QCE; TCE + exposed to B-cell maturation antigen targeted drug) were also analyzed. Index date was defined as LOT start date after each exposure definitions. Descriptive statistics were reported for patient characteristics and treatment patterns. Clinical outcomes such as time to treatment discontinuation or death (TTD), and time to next treatment or death (TTNT) were estimated using the Kaplan-Meier method. Here we reported data for TCE and TCE with 4+ prior PLs; data for QCE cohort will be presented in the future.
Results: A total of 1,704 TCE patients were included, among whom 1,072 had 4+ PLs. For TCE and TCE with 4+ PLs cohorts, the mean (median) ages were 64.6 (64.0) and 64.9 (64.0), and 46.6% and 47.4% were females, respectively. The mean (median) number of prior LOTs before index date were 3.9 (4.0) and 4.7 (4.0), respectively. Most patients who were TCE and TCE with 4+ PLs were exposed to daratumumab (D; 99.9% and 99.8%), lenalidomide (85.6% and 86.4 %), and bortezomib (84.2 % and 83.0%) before index date. The most common post-TCE treatments were pomalidomide (P)- (36.0%), D- (35.0%), and carfilzomib (K)- (33.7%) based regimens. Similarly, the most common post-TCE with 4+ PLs treatments were P- (33.8%), K- (33.8%), and D- (30.5%) based regimens. At the regimen level, D+P±dexamethasone was the most commonly used post-index regimen (8.0% and 6.7% for TCE and TCE with 4+ PLs, respectively). The median TTD (months) were 5.8 (95% CI 5.4-6.5) for TCE and 5.1 (95% CI 4.8-5.6) for TCE with 4+ PLs, while the median TTNT (months) were 8.4 (95% CI 7.9-9.4) for TCE and 7.1 (95% CI 6.7-7.8) for TCE with 4+ PLs.
Conclusions: These findings demonstrate that in the real-world, patients have limited treatment options after TCE and are often retreated with the same therapies or therapies in the same classes. Patients who were TCE discontinued treatment and moved on to next treatment shortly after initial treatment. These outcomes were even shorter for those with 4+ PLs. The findings highlight the continued need for effective treatments for heavily treated patients with MM.
