Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-298: Retrospective study of treatment patterns and clinical outcomes by race in patients with triple-class-exposed multiple myeloma treated in a real-world setting
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST
.jpg)
ASTER MECHE, MPH
RWE SCIENTIST
PFIZER INC, United States
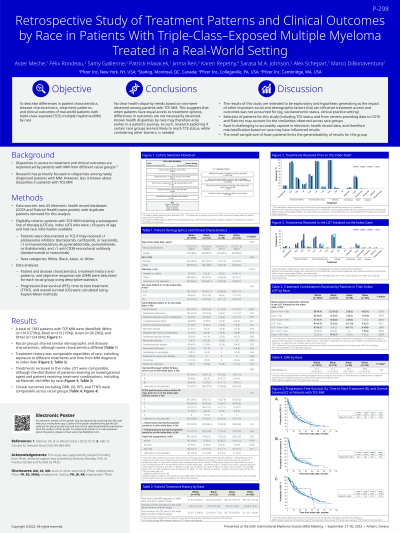
Introduction: Disparities in access to treatment and clinical outcomes are experienced by multiple myeloma (MM) patients from different racial groups. The objective of this study was to describe differences in treatment patterns and clinical outcomes of real-world (RW) triple-class-exposed (TCE) MM patients (i.e., exposed to ≥1 PI, ≥1 IMiD, ≥1 anti-CD38) by race.
Methods: Data from two US electronic health record databases (COTA and Flatiron Health) were pooled with duplicate patients removed for this analysis. TCE MM patients initiating a subsequent line of therapy (LOT) (i.e., index LOT) following documentation of exposure to all three classes of drug, who were ≥18 years, and had race information captured within these databases were identified. Patients were categorized as White, Black, Asian, or Other race. Patient and disease characteristics, treatment history and patterns, and clinical outcomes (i.e., response, progression, treatment switch, and death) were described for each racial group using descriptive statistics. Progression-free survival (PFS), time to next treatment (TTNT), and overall survival (OS) were calculated using Kaplan-Meier methods.
Results: A total of 1,383 patients were identified (White 1,010 (73%); Black 213 (15%); Asian 36 (3%); Other 124 (9%)). Patient characteristics were similar though Other patients were more likely to identify as Hispanic (41% vs 2-8%, p<.05) and the distribution of some comorbidities also differed (e.g., renal disease: White 10%, Black 17%, Asian 14%, Other 14%, p<.05). Disease characteristics and treatment history were also comparable regardless of race, including exposure to different treatments (e.g., stem cell transplant 47-53%, p=.38) and time from MM diagnosis to index LOT (36.3-41.5 median (m) months, p=.62). However, a significantly higher proportion of Asian patients had the t(4;14) cytogenetic marker (25% vs 8-11%, p<.05). Treatments received in the index LOT were comparable, though White patients were more likely to receive an investigational agent (5% vs 0-2%, p<.05) and Asian patients were more likely to receive treatment combinations including carfilzomib (50% vs 27-31%, p<.05). Response rates did not differ significantly based on race (White 27%, Black 27%, Asian 44%, Other 30%, p=.15). Time-to-event outcome results (months) were as follows: mPFS - White 9.9, Black 8.3, Asian 15.9, Other 12.7; mTTNT – White 7.6, Black 8.9, Asian 10.9, Other 7.8; mOS – White 21.1, Black 17.4, Asian 37.5, Other 27.4.
Conclusions: No clear health disparity trends were observed among TCE MM patients based on race. This suggests that when patients have equal access to treatment options, differences in outcomes are not necessarily observed. Known health disparities by race may therefore arise earlier in a patient’s journey. As such, research exploring if certain race groups are less likely to reach TCE status, while considering other barriers, is needed.
Methods: Data from two US electronic health record databases (COTA and Flatiron Health) were pooled with duplicate patients removed for this analysis. TCE MM patients initiating a subsequent line of therapy (LOT) (i.e., index LOT) following documentation of exposure to all three classes of drug, who were ≥18 years, and had race information captured within these databases were identified. Patients were categorized as White, Black, Asian, or Other race. Patient and disease characteristics, treatment history and patterns, and clinical outcomes (i.e., response, progression, treatment switch, and death) were described for each racial group using descriptive statistics. Progression-free survival (PFS), time to next treatment (TTNT), and overall survival (OS) were calculated using Kaplan-Meier methods.
Results: A total of 1,383 patients were identified (White 1,010 (73%); Black 213 (15%); Asian 36 (3%); Other 124 (9%)). Patient characteristics were similar though Other patients were more likely to identify as Hispanic (41% vs 2-8%, p<.05) and the distribution of some comorbidities also differed (e.g., renal disease: White 10%, Black 17%, Asian 14%, Other 14%, p<.05). Disease characteristics and treatment history were also comparable regardless of race, including exposure to different treatments (e.g., stem cell transplant 47-53%, p=.38) and time from MM diagnosis to index LOT (36.3-41.5 median (m) months, p=.62). However, a significantly higher proportion of Asian patients had the t(4;14) cytogenetic marker (25% vs 8-11%, p<.05). Treatments received in the index LOT were comparable, though White patients were more likely to receive an investigational agent (5% vs 0-2%, p<.05) and Asian patients were more likely to receive treatment combinations including carfilzomib (50% vs 27-31%, p<.05). Response rates did not differ significantly based on race (White 27%, Black 27%, Asian 44%, Other 30%, p=.15). Time-to-event outcome results (months) were as follows: mPFS - White 9.9, Black 8.3, Asian 15.9, Other 12.7; mTTNT – White 7.6, Black 8.9, Asian 10.9, Other 7.8; mOS – White 21.1, Black 17.4, Asian 37.5, Other 27.4.
Conclusions: No clear health disparity trends were observed among TCE MM patients based on race. This suggests that when patients have equal access to treatment options, differences in outcomes are not necessarily observed. Known health disparities by race may therefore arise earlier in a patient’s journey. As such, research exploring if certain race groups are less likely to reach TCE status, while considering other barriers, is needed.
