Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-325: Standard of Care (SOC) Outcomes in the Last 3 Years in Patients With Triple-Class Exposed (TCE) Relapsed/Refractory Multiple Myeloma (RRMM): The First Pooled Analysis of LocoMMotion and MoMMent Trials
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST

Katja Weisel, MD (she/her/hers)
Deputy Director
University Medical Center of Hamburg-Eppendorf, Hamburg, Germany
Hamburg, Germany
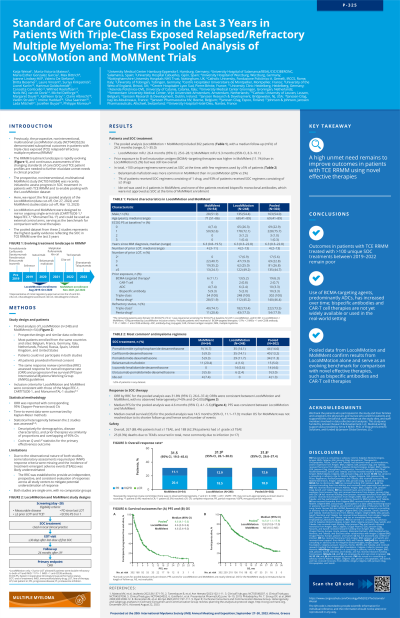
Introduction: The prospective, non-interventional, multinational LocoMMotion study (NCT04035226) demonstrated suboptimal outcomes in patients (pts) with TCE RRMM (Mateos, Leukemia 2022; data cut-off, May 21, 2021). As a complement to LocoMMotion, the prospective, non-interventional, multinational MoMMent study (NCT05160584) was recently initiated to assess the evolving SOC in pts with TCE RRMM. We report the first pooled analysis of the LocoMMotion (final) and MoMMent studies (data cut-off, Oct 27, 2022).
Methods: Data were pooled from LocoMMotion, with median follow-up (mFU) of 26.4 months (mo; range, 0.1–35.0) in 248 pts enrolled Aug 2019–Oct 2020, and MoMMent, with mFU of 5.1 mo (range, 0.4–10.9) in 54 pts enrolled Nov 2021–Jul 2022. Both studies have similar designs; statistical heterogeneity was investigated using Cochran Q and I-square. Eligible pts received ≥3 prior lines of therapy (LOT; LocoMMotion allowed < 3 prior LOT if pts were double refractory to a PI and IMiD), were TCE, had measurable disease and documented progressive disease since their last LOT, and had an ECOG performance status (PS) score of 0 or 1 at screening. All pts provided informed consent. The primary endpoint was overall response rate (ORR), evaluated per IMWG criteria by the same review committee. Continuous variables were summarized using descriptive statistics, and ORR was reported with 95% exact CIs. Time-to-event data were summarized by Kaplan-Meier methods.
Results: Pooled analysis included 302 pts with a mFU of 24.4 mo (range, 0.1–35.0). At baseline, median age was 69 years (y), 54% of pts were male, 75.7% had an ECOG PS of 1, and median time since diagnosis was 6.3 y. Pts received a median of 4 prior LOT (range, 2–13), 73.5% were triple-class refractory, and 17.9% were penta-drug refractory. Prior exposure to BCMA-targeting therapies was higher in MoMMent vs LocoMMotion (11% vs 5%). Overall, 102 unique regimens were used as SOC, and 63.9% of pts received regimens comprising ≥3 drugs. Belantamab mafodotin (22% vs 3%) and idecabtagene vicleucel (6% vs 0%) were more common in MoMMent vs LocoMMotion. In the pooled analysis, ORR was 30.8% (95% CI, 25.6–36.3), median progression-free survival (mPFS) was 4.9 mo (95% CI, 4.2–5.7), and median overall survival was 13.83 mo (95% CI, 10.8–16.9). In MoMMent, ORR was 25.9% (95% CI, 15.0–39.7) and mPFS was 4.9 mo (95% CI, 3.1–6.3), consistent with the LocoMMotion results. Overall, 264 (87.4%) pts reported ≥1 any grade treatment-emergent adverse event (TEAE), with 187 (61.9%) reporting ≥1 grade ≥3 TEAE. 23 (7.6%) deaths due to TEAEs occurred on study, mostly due to infection (n=15).
Conclusions: These initial results suggest that outcomes in pts with TCE RRMM remain poor. A high unmet need remains for pts with TCE RRMM, as evidenced by the observation that bispecific antibody and CAR-T cell therapies are not yet widely utilized. Increased adoption of these novel immunotherapies into SOC is key to improving outcomes. Additional MoMMent data at 9.2 mo mFU will be presented.
Methods: Data were pooled from LocoMMotion, with median follow-up (mFU) of 26.4 months (mo; range, 0.1–35.0) in 248 pts enrolled Aug 2019–Oct 2020, and MoMMent, with mFU of 5.1 mo (range, 0.4–10.9) in 54 pts enrolled Nov 2021–Jul 2022. Both studies have similar designs; statistical heterogeneity was investigated using Cochran Q and I-square. Eligible pts received ≥3 prior lines of therapy (LOT; LocoMMotion allowed < 3 prior LOT if pts were double refractory to a PI and IMiD), were TCE, had measurable disease and documented progressive disease since their last LOT, and had an ECOG performance status (PS) score of 0 or 1 at screening. All pts provided informed consent. The primary endpoint was overall response rate (ORR), evaluated per IMWG criteria by the same review committee. Continuous variables were summarized using descriptive statistics, and ORR was reported with 95% exact CIs. Time-to-event data were summarized by Kaplan-Meier methods.
Results: Pooled analysis included 302 pts with a mFU of 24.4 mo (range, 0.1–35.0). At baseline, median age was 69 years (y), 54% of pts were male, 75.7% had an ECOG PS of 1, and median time since diagnosis was 6.3 y. Pts received a median of 4 prior LOT (range, 2–13), 73.5% were triple-class refractory, and 17.9% were penta-drug refractory. Prior exposure to BCMA-targeting therapies was higher in MoMMent vs LocoMMotion (11% vs 5%). Overall, 102 unique regimens were used as SOC, and 63.9% of pts received regimens comprising ≥3 drugs. Belantamab mafodotin (22% vs 3%) and idecabtagene vicleucel (6% vs 0%) were more common in MoMMent vs LocoMMotion. In the pooled analysis, ORR was 30.8% (95% CI, 25.6–36.3), median progression-free survival (mPFS) was 4.9 mo (95% CI, 4.2–5.7), and median overall survival was 13.83 mo (95% CI, 10.8–16.9). In MoMMent, ORR was 25.9% (95% CI, 15.0–39.7) and mPFS was 4.9 mo (95% CI, 3.1–6.3), consistent with the LocoMMotion results. Overall, 264 (87.4%) pts reported ≥1 any grade treatment-emergent adverse event (TEAE), with 187 (61.9%) reporting ≥1 grade ≥3 TEAE. 23 (7.6%) deaths due to TEAEs occurred on study, mostly due to infection (n=15).
Conclusions: These initial results suggest that outcomes in pts with TCE RRMM remain poor. A high unmet need remains for pts with TCE RRMM, as evidenced by the observation that bispecific antibody and CAR-T cell therapies are not yet widely utilized. Increased adoption of these novel immunotherapies into SOC is key to improving outcomes. Additional MoMMent data at 9.2 mo mFU will be presented.
