Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-299: Survival Outcomes in Older Patients with Relapsed/Refractory Multiple Myeloma Treated with Either IMiD- or Non-IMiD-Based Regimens After Triple-Class Exposure in the PREAMBLE Registry
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST

Philippe Moreau, MD
Head of Hematology
University Hospital Hôtel-Dieu, Nantes, France
Nantes, Pays de la Loire, France
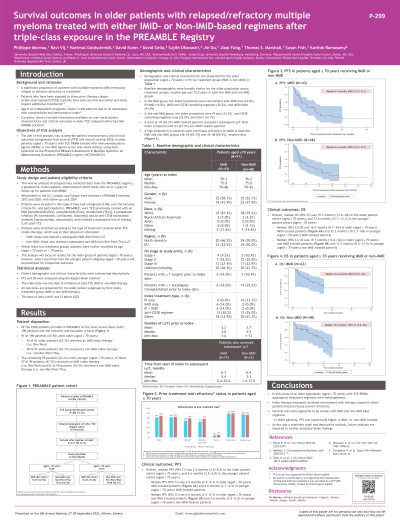
Introduction: A significant proportion of patients with multiple myeloma (MM) eventually relapse or become refractory to treatment. Age is an independent prognostic factor in MM, but there is limited information on real-world treatment patterns and clinical outcomes in older patients with relapsed/refractory MM (RRMM) who have been exposed to three prior therapy classes (triple-class exposed [TCE]). The aim of this analysis was to describe the patient characteristics and outcomes (progression-free survival [PFS] and overall survival [OS]) in older patients with TCE RRMM treated with immunomodulatory agents (IMiDs) or non-IMiD agents in the real-world setting.
Methods: Prospectively collected data were extracted from the multicenter Prospective REsearch Assessment in Multiple Myeloma: An oBservational Evaluation (PREAMBLE) registry, which enrolled patients with newly diagnosed MM and RRMM in Europe and the US from 2012 to 2020. Included patients were ≥70 years of age, TCE (previously treated with an IMiD [lenalidomide (Rev), pomalidomide (Pom), thalidomide (Tha)], an anti-CD38 antibody, and a proteasome inhibitor [PI]), and started a subsequent IMiD (Rev/Pom) or non-IMiD (non-Rev/Pom/Tha) line of therapy at their physician’s discretion. All analyses were descriptive; Kaplan-Meier curves were used for PFS and OS analyses. Index date was the date of initiation of post-TCE IMiD or non-IMiD therapy.
Results: Among 190 TCE patients who initiated a subsequent line of therapy, 91 patients were ≥70 years of age (median age 75 years). At index, 43 of these patients (47.3%) received an IMiD regimen and 48 (52.7%) received a non-IMiD regimen. Baseline demographics were broadly similar between groups. A high proportion of patients were previously refractory to IMiDs in both the IMiD and non-IMiD groups (36/43 [83.7%] and 43/48 [89.6%], respectively). In the IMiD group, the index treatments were: retreatment with IMiD only (14.0%), IMiD+PI (14.0%), IMiD + anti-CD38 (30.2%), and IMiD + other (41.9%). In the non-IMiD group, the index treatments were: PI only (33.3%), anti-CD38 containing regimens (25.0%), and other (41.7%). A total of 19 (44.2%) IMiD-treated patients received a subsequent line of therapy after index compared with 23 (47.9%) non-IMiD treated patients. Overall, the median (95% CI) PFS in this group of patients aged ≥70 years was 5.2 (3.0–8.3) months, with 5.9 (2.9–9.3) months in IMiD-treated patients compared with 4.6 (2.3–8.3) months in non-IMiD treated patients. The overall median (95% CI) OS was 19.7 (13.0–NA) months – 16.0 (8.7–NA) in IMiD-treated patients compared with 19.7 (13.0–NA) in non-IMiD treated patients.
Conclusions: In this study of an older population with TCE RRMM, subsequent treatment regimens were heterogeneous. Survival outcomes appeared to be similar with IMiD- and non-IMiD–based regimens. As this was a relatively small and descriptive study, future analyses are required to further elucidate these findings.
Methods: Prospectively collected data were extracted from the multicenter Prospective REsearch Assessment in Multiple Myeloma: An oBservational Evaluation (PREAMBLE) registry, which enrolled patients with newly diagnosed MM and RRMM in Europe and the US from 2012 to 2020. Included patients were ≥70 years of age, TCE (previously treated with an IMiD [lenalidomide (Rev), pomalidomide (Pom), thalidomide (Tha)], an anti-CD38 antibody, and a proteasome inhibitor [PI]), and started a subsequent IMiD (Rev/Pom) or non-IMiD (non-Rev/Pom/Tha) line of therapy at their physician’s discretion. All analyses were descriptive; Kaplan-Meier curves were used for PFS and OS analyses. Index date was the date of initiation of post-TCE IMiD or non-IMiD therapy.
Results: Among 190 TCE patients who initiated a subsequent line of therapy, 91 patients were ≥70 years of age (median age 75 years). At index, 43 of these patients (47.3%) received an IMiD regimen and 48 (52.7%) received a non-IMiD regimen. Baseline demographics were broadly similar between groups. A high proportion of patients were previously refractory to IMiDs in both the IMiD and non-IMiD groups (36/43 [83.7%] and 43/48 [89.6%], respectively). In the IMiD group, the index treatments were: retreatment with IMiD only (14.0%), IMiD+PI (14.0%), IMiD + anti-CD38 (30.2%), and IMiD + other (41.9%). In the non-IMiD group, the index treatments were: PI only (33.3%), anti-CD38 containing regimens (25.0%), and other (41.7%). A total of 19 (44.2%) IMiD-treated patients received a subsequent line of therapy after index compared with 23 (47.9%) non-IMiD treated patients. Overall, the median (95% CI) PFS in this group of patients aged ≥70 years was 5.2 (3.0–8.3) months, with 5.9 (2.9–9.3) months in IMiD-treated patients compared with 4.6 (2.3–8.3) months in non-IMiD treated patients. The overall median (95% CI) OS was 19.7 (13.0–NA) months – 16.0 (8.7–NA) in IMiD-treated patients compared with 19.7 (13.0–NA) in non-IMiD treated patients.
Conclusions: In this study of an older population with TCE RRMM, subsequent treatment regimens were heterogeneous. Survival outcomes appeared to be similar with IMiD- and non-IMiD–based regimens. As this was a relatively small and descriptive study, future analyses are required to further elucidate these findings.
