Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-283: Systematic literature review of prognostic factors for relapsed/refractory multiple myeloma
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST

Shaji K. Kumar, MD
Professor of Medicine/Consultant
Mayo Clinic, Rochester, MN, US
Rochester, Minnesota, United States
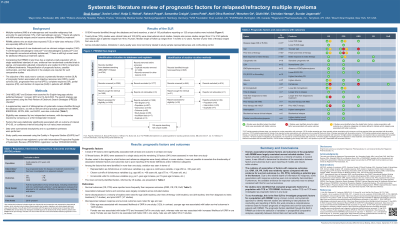
Introduction: Patients with relapsed and/or refractory multiple myeloma (RRMM) have a poor prognosis that is further reduced when exposed to multiple therapies. Although several studies have identified factors prognostic of outcomes in patients with RRMM, an up-to-date synthesis is lacking. A systematic and evidence-based approach to identify relevant prognostic factors to support RRMM research is needed in a rapidly changing treatment landscape. Our objective was to conduct a systematic literature review (SLR) of prognostic factors associated with response (objective, complete, and partial response rates, duration of response) and survival (overall and progression-free survival) outcomes in patients with RRMM.
Methods: Ovid MEDLINE and Embase were searched for clinical trials and observational studies published between January 1, 2016 and April 14, 2022. Eligible studies included RRMM patients and an assessment of prognostic significance of any factor on an outcome of interest via multivariate analysis. Two independent reviewers assessed eligibility, with discrepancies resolved by consensus or a third independent reviewer. Data were extracted using standardized templates. Factors statistically significantly associated with an outcome of interest (p < 0.05, or confidence interval excluding the null value) were extracted. Study quality was assessed using the Quality in Prognosis Studies (QUIPS) tool. Data were summarized descriptively.
Results: Of 5,349 records identified, 130 records reporting on 125 unique studies (23 clinical trials and 102 observational studies) were included. The most common limitations in study quality were related to sample representativeness and control of confounders.
Ninety-seven factors were significantly associated with at least one outcome in at least one study. The most commonly identified factors were disease stage (n = 27 studies), age (n = 20), prior lines of therapy (n = 20), best response to index therapy (n = 20), cytogenetic risk (n = 19), lactate dehydrogenase (LDH; n = 12), extramedullary disease/plasmacytoma (EMP) (n = 12), and performance status (PS) (n = 10). Worse survival was associated with higher disease stage, older age, more prior lines of therapy, poorer response, high-risk cytogenetics, elevated LDH levels, EMP presence, and worse PS. Worse response was associated with higher disease stage, younger age, more prior lines of therapy, high-risk cytogenetics, and worse PS. Associations between factors and outcomes were largely consistent across studies, although conflicting associations were noted in < 10% of studies; in some studies, poor reporting limited the ability to ascertain the direction of associations.
Conclusions: To our best knowledge, this is the first SLR to investigate prognostic factors for an RRMM population. This work provides a comprehensive evidence base for factors prognostic of response and survival outcomes in patients with RRMM.
Methods: Ovid MEDLINE and Embase were searched for clinical trials and observational studies published between January 1, 2016 and April 14, 2022. Eligible studies included RRMM patients and an assessment of prognostic significance of any factor on an outcome of interest via multivariate analysis. Two independent reviewers assessed eligibility, with discrepancies resolved by consensus or a third independent reviewer. Data were extracted using standardized templates. Factors statistically significantly associated with an outcome of interest (p < 0.05, or confidence interval excluding the null value) were extracted. Study quality was assessed using the Quality in Prognosis Studies (QUIPS) tool. Data were summarized descriptively.
Results: Of 5,349 records identified, 130 records reporting on 125 unique studies (23 clinical trials and 102 observational studies) were included. The most common limitations in study quality were related to sample representativeness and control of confounders.
Ninety-seven factors were significantly associated with at least one outcome in at least one study. The most commonly identified factors were disease stage (n = 27 studies), age (n = 20), prior lines of therapy (n = 20), best response to index therapy (n = 20), cytogenetic risk (n = 19), lactate dehydrogenase (LDH; n = 12), extramedullary disease/plasmacytoma (EMP) (n = 12), and performance status (PS) (n = 10). Worse survival was associated with higher disease stage, older age, more prior lines of therapy, poorer response, high-risk cytogenetics, elevated LDH levels, EMP presence, and worse PS. Worse response was associated with higher disease stage, younger age, more prior lines of therapy, high-risk cytogenetics, and worse PS. Associations between factors and outcomes were largely consistent across studies, although conflicting associations were noted in < 10% of studies; in some studies, poor reporting limited the ability to ascertain the direction of associations.
Conclusions: To our best knowledge, this is the first SLR to investigate prognostic factors for an RRMM population. This work provides a comprehensive evidence base for factors prognostic of response and survival outcomes in patients with RRMM.
