QoL and Patient-Reported Outcome and Supportive Care
Poster Session 3
P-464: Treatment Decision-Making in Patients Diagnosed With Multiple Myeloma
Friday, September 29, 2023
1:15 PM - 2:15 PM EEST
.jpg)
Doris K. Hansen, MD
Assistant Professor
Moffiitt Cancer Center
Tampa, Florida, United States
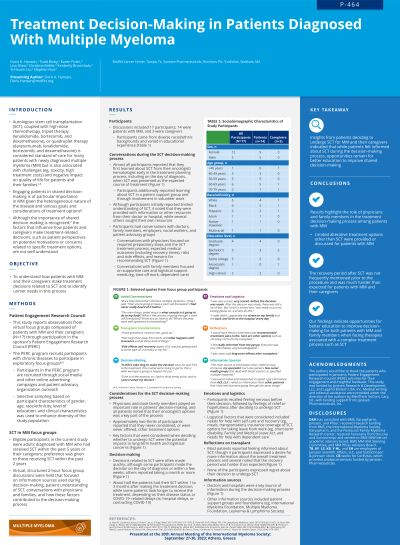
Introduction: Shared decision-making is an important component in patient-centered healthcare, particularly for patients with multiple myeloma (MM) seeking individualized treatment options. In this study, we assessed how patients and caregivers make decisions related to stem-cell transplantation (SCT) and identified unmet needs in this process.
Methods: Adult patients diagnosed with MM who received SCT within the past 5 years or their caregivers were recruited to participate in virtual structured 2-hour focus group discussions through involvement in a Patient Engagement Research Council focused on experiences with SCT. Discussions focused on information sources, patient understanding of SCT, conversations with doctors and families, and how these factors contributed to decision-making.
Results: Discussions included 17 participants (14 patients, 3 caregivers). Approximately half of all participants (n=9, 53%) were < 60 years old, and 70% were female (n=12). Participants came from diverse racial/ethnic backgrounds (White, n=5; Black, n=6; other ethnic groups, n=6) and varied in educational experience (postgraduate, n=4; college graduate or some college, n=11; high school, n=2). Almost all participants learned about SCT from their oncologist or hematologist early in treatment planning, when SCT was presented as the expected treatment course. Although around half of the participants recalled initially having limited knowledge of SCT, many sought information from outside organizations (eg, foundations/societies, patient support groups); some received resources from their doctor. Key factors considered before deciding to proceed with SCT included long-term health impacts, side effects, and logistical or financial concerns. Participants spoke with their doctors about the SCT treatment process and potential risks and outcomes; family members were consulted regarding caregiving or logistical support needs. Decisions related to SCT were often made quickly; 2 patients made the decision on the day of diagnosis or within a few weeks. Approximately two-thirds of participants reported that they never considered, or were never offered, other treatment options. Participants recalled feeling nervous before their decision, followed by feelings of relief or hopefulness after deciding to undergo SCT. Four participants desired more information about the SCT process, particularly the recovery period, and 2 participants recalled feeling overwhelmed during decision-making. However, participants overall felt that they were adequately informed about SCT, and none regretted their decision to undergo SCT.
Conclusions: Patients deciding to undergo SCT for MM drew on multiple information sources during the decision-making process but relied heavily on doctors’ recommendations. Shared decision-making between patients, families, and providers—including education and discussion of alternative options and recovery—is important for patients facing a complex treatment process.
Methods: Adult patients diagnosed with MM who received SCT within the past 5 years or their caregivers were recruited to participate in virtual structured 2-hour focus group discussions through involvement in a Patient Engagement Research Council focused on experiences with SCT. Discussions focused on information sources, patient understanding of SCT, conversations with doctors and families, and how these factors contributed to decision-making.
Results: Discussions included 17 participants (14 patients, 3 caregivers). Approximately half of all participants (n=9, 53%) were < 60 years old, and 70% were female (n=12). Participants came from diverse racial/ethnic backgrounds (White, n=5; Black, n=6; other ethnic groups, n=6) and varied in educational experience (postgraduate, n=4; college graduate or some college, n=11; high school, n=2). Almost all participants learned about SCT from their oncologist or hematologist early in treatment planning, when SCT was presented as the expected treatment course. Although around half of the participants recalled initially having limited knowledge of SCT, many sought information from outside organizations (eg, foundations/societies, patient support groups); some received resources from their doctor. Key factors considered before deciding to proceed with SCT included long-term health impacts, side effects, and logistical or financial concerns. Participants spoke with their doctors about the SCT treatment process and potential risks and outcomes; family members were consulted regarding caregiving or logistical support needs. Decisions related to SCT were often made quickly; 2 patients made the decision on the day of diagnosis or within a few weeks. Approximately two-thirds of participants reported that they never considered, or were never offered, other treatment options. Participants recalled feeling nervous before their decision, followed by feelings of relief or hopefulness after deciding to undergo SCT. Four participants desired more information about the SCT process, particularly the recovery period, and 2 participants recalled feeling overwhelmed during decision-making. However, participants overall felt that they were adequately informed about SCT, and none regretted their decision to undergo SCT.
Conclusions: Patients deciding to undergo SCT for MM drew on multiple information sources during the decision-making process but relied heavily on doctors’ recommendations. Shared decision-making between patients, families, and providers—including education and discussion of alternative options and recovery—is important for patients facing a complex treatment process.
