Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-310: Treatment Preferences Among Triple-class Exposed Patients With Relapsed/Refractory Multiple Myeloma in the United States (US), United Kingdom (UK), and Germany (DE): a Discrete Choice Experiment
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST
.jpg)
Paula Rodríguez-Otero, MD, PhD (she/her/hers)
Associate Professor
Clínica Universidad de Navarra, CIMA, CIBERONC, IDISNA, Pamplona, Spain
Pamplona, Navarra, Spain
Introduction: Front line therapies for multiple myeloma (MM) comprise 3 treatment classes: immunomodulators, proteasome inhibitors, and anti-CD38 antibodies. Few treatment options are available for patients who relapse or are refractory to all 3 classes (triple-class exposed [TCE]), and prognoses are poor. Chimeric antigen receptor (CAR) T cell therapies offer new options for treating TCE patients with relapsed/refractory MM (RRMM). However, patient preferences for CAR T therapy attributes are poorly understood. This study aimed to quantify preferences for attributes relating to standard multi-cycle treatments and CAR T therapy in patients with TCE RRMM.
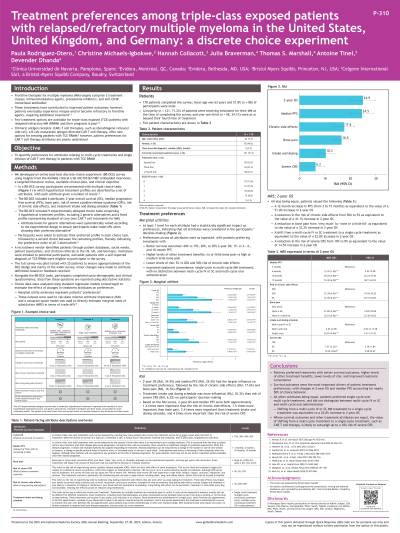
Methods: An online survey and best–best discrete choice experiment (BB-DCE), was developed based on clinical trial interviews, a literature review, and clinical expertise. The BB-DCE included 6 treatment attributes: 2-year overall survival (OS), median progression-free survival (PFS), bone pain, risk of severe cytokine release syndrome (sCRS), risk of any mild-to-moderate chronic side effects, and dosing schedule reflecting two multi-cycle (oral and subcutaneous or intravenous) and one single-cycle options. Each of the 9 choice tasks consisted of 3 treatment profiles; attribute levels presented in 2 profiles varied according to an experimental design, and 1 fixed profile aligned with a standard multi-cycle treatment. Patients selected the most preferred profile out of 3, then the most preferred from the remaining 2. Adults (≥18 years of age) with self-reported TCE RRMM were eligible to complete the survey. Choice data were analyzed using standard regression models (mixed logit) to estimate preference weights. Relative attribute importance (RAI) scores were calculated, and attribute trade-offs were estimated using a valuation space model with OS as numéraire.
Results: A total of 170 TCE patients (UK: n=30, US: n=87, DE: n=53) completed the BB-DCE. Mean age was 63 years; 51.8% (n=88) were male. At the time of the study, most patients were receiving MM treatment (n=121).
Across attributes, changes in 2-year OS had the largest influence on treatment preferences (24.9%), followed by PFS (24.5%), chronic side effects (17.6%), bone pain (16.5%), and dosing schedule (10.3%), and risk of sCRS (6.2%). All else being equal, patients preferred single-cycle over multi-cycle treatment (oral or SC/IV. OS and PFS were both 4 times more important than the risk of sCRS.
The additional value that patients placed on a treatment offering a 12-month increase in PFS (from 3 to 15 months) was equivalent to the value of a 51% increase in OS. Patients valued shifting from a multi-cycle IV or SC treatment to a single-cycle treatment as equivalent to a 23% increase in 2-year OS.
Conclusions: Patients’ preferences for RRMM treatments were driven by survival outcomes. All else being equal, the value that patients place on a single-cycle treatment such as CAR T cell therapy is likely to outweigh up to a 10% risk of sCRS.
Methods: An online survey and best–best discrete choice experiment (BB-DCE), was developed based on clinical trial interviews, a literature review, and clinical expertise. The BB-DCE included 6 treatment attributes: 2-year overall survival (OS), median progression-free survival (PFS), bone pain, risk of severe cytokine release syndrome (sCRS), risk of any mild-to-moderate chronic side effects, and dosing schedule reflecting two multi-cycle (oral and subcutaneous or intravenous) and one single-cycle options. Each of the 9 choice tasks consisted of 3 treatment profiles; attribute levels presented in 2 profiles varied according to an experimental design, and 1 fixed profile aligned with a standard multi-cycle treatment. Patients selected the most preferred profile out of 3, then the most preferred from the remaining 2. Adults (≥18 years of age) with self-reported TCE RRMM were eligible to complete the survey. Choice data were analyzed using standard regression models (mixed logit) to estimate preference weights. Relative attribute importance (RAI) scores were calculated, and attribute trade-offs were estimated using a valuation space model with OS as numéraire.
Results: A total of 170 TCE patients (UK: n=30, US: n=87, DE: n=53) completed the BB-DCE. Mean age was 63 years; 51.8% (n=88) were male. At the time of the study, most patients were receiving MM treatment (n=121).
Across attributes, changes in 2-year OS had the largest influence on treatment preferences (24.9%), followed by PFS (24.5%), chronic side effects (17.6%), bone pain (16.5%), and dosing schedule (10.3%), and risk of sCRS (6.2%). All else being equal, patients preferred single-cycle over multi-cycle treatment (oral or SC/IV. OS and PFS were both 4 times more important than the risk of sCRS.
The additional value that patients placed on a treatment offering a 12-month increase in PFS (from 3 to 15 months) was equivalent to the value of a 51% increase in OS. Patients valued shifting from a multi-cycle IV or SC treatment to a single-cycle treatment as equivalent to a 23% increase in 2-year OS.
Conclusions: Patients’ preferences for RRMM treatments were driven by survival outcomes. All else being equal, the value that patients place on a single-cycle treatment such as CAR T cell therapy is likely to outweigh up to a 10% risk of sCRS.
