Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-287: Isatuximab Plus Pomalidomide and Dexamethasone in Patients With Relapsed and/or Refractory Multiple Myeloma in Real Life Context in France: IMAGE Subgroup Analysis Based on Subgroups of Interest
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST

Xavier P. Leleu, MD, PhD (he/him/his)
Head of Myeloma Clinic and Head of Department of Haematology
Hospital La Mileterie, Poitiers, France
Poitiers, United States
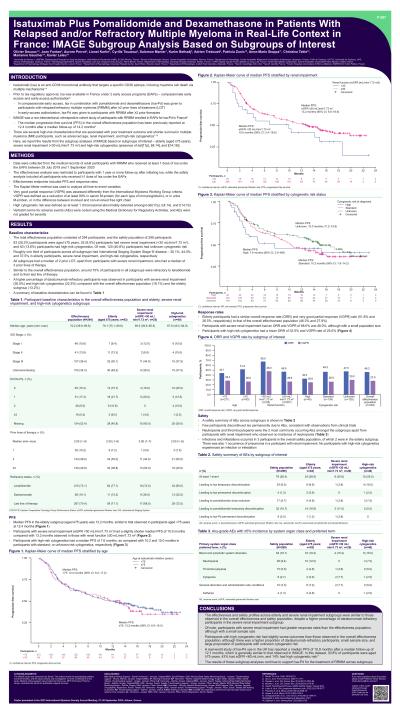
Introduction: IMAGE was a non-interventional, retrospective cohort study of patients (pts) with relapsed/refractory multiple myeloma (RRMM) enrolled in early access programs (EAPs) for isatuximab with pomalidomide and dexamethasone (Isa-Pd) in France. The median progression-free survival (mPFS) in the overall effectiveness population was 12.4 months (mo) after a median follow-up of 14.2 mo. Here, we report results from the subgroup analysis of the IMAGE study based on subgroups of interest – elderly (aged ≥75), severe renal impairment ( < 30 mL/min/1.73m2) and high-risk (HR) cytogenetics.
Methods: IMAGE used medical records of adult pts with RRMM who received ≥1 dose of Isa under EAPs. Effectiveness analysis was restricted to pts with ≥1 year of follow-up after Isa initiation, while safety analysis included all pts who received ≥1 dose of Isa. HR cytogenetics was the detection of at least one of the following: del(17p), t(4;14), and t(14;16). PFS was defined as the time from start of Isa-Pd to date of disease progression, as reported in the medical record, or death. Verbatim terms for adverse events (AEs) were coded using the Medical Dictionary for Regulatory Activities, and AEs were not graded for severity.
Results: The total effectiveness population was 294, while safety population was 299. 83 pts were aged ≥75, 25 pts had renal function < 30 mL/min/1.73m2, and 40 pts had HR cytogenetics. 120 pts had unknown cytogenetic risk.
Majority of pts across all subgroups had International Staging System Stage III disease, and all subgroups had a median 2 prior lines of therapy, except for pts with renal impairment who had a median 3 prior lines of therapy. Similar to the overall effectiveness population, around 70% of pts in all subgroups were refractory to lenalidomide and their last line of therapy.
The mPFS was 13.2 (95% CI: 6.8-15.0) mo, 10.0 (95% CI: 2.4-18.6) mo, and 7.6 (95% CI: 2.8-Not reached) mo in pts aged ≥75, with severe renal impairment, and HR cytogenetics, respectively. Overall response and very good partial response rates were 51.8% and 26.5% in elderly pts, 68.0% and 48.0% in pts with severe renal impairment, and 32.5% and 25.0% in pts with HR cytogenetics. In the overall effectiveness population, ORR and VGPR were 46.3% and 27.9%.
28.9% of elderly, 25.0% of HR cytogenetics, and 30.8% of renal impaired pts had at least one AE. 1 elderly pt and 1 pt with HR cytogenetics had an AE leading to permanent discontinuation of Isa. The incidence of neutropenia was 8.3%, 0%, and 7.5% in elderly, renal impaired, and HR cytogenetics pts. Infections and infestations occurred in 3 pts in the overall safety population — 2 in elderly, 1 in renal impaired, and 0 in HR cytogenetics pts.
Conclusions: The effectiveness and safety profiles across elderly, renal impaired, and HR cytogenetics subgroups were similar to those in the overall effectiveness population. The results of this subgroup analyses continue to support Isa-Pd for treatment of RRMM across subgroups.
Methods: IMAGE used medical records of adult pts with RRMM who received ≥1 dose of Isa under EAPs. Effectiveness analysis was restricted to pts with ≥1 year of follow-up after Isa initiation, while safety analysis included all pts who received ≥1 dose of Isa. HR cytogenetics was the detection of at least one of the following: del(17p), t(4;14), and t(14;16). PFS was defined as the time from start of Isa-Pd to date of disease progression, as reported in the medical record, or death. Verbatim terms for adverse events (AEs) were coded using the Medical Dictionary for Regulatory Activities, and AEs were not graded for severity.
Results: The total effectiveness population was 294, while safety population was 299. 83 pts were aged ≥75, 25 pts had renal function < 30 mL/min/1.73m2, and 40 pts had HR cytogenetics. 120 pts had unknown cytogenetic risk.
Majority of pts across all subgroups had International Staging System Stage III disease, and all subgroups had a median 2 prior lines of therapy, except for pts with renal impairment who had a median 3 prior lines of therapy. Similar to the overall effectiveness population, around 70% of pts in all subgroups were refractory to lenalidomide and their last line of therapy.
The mPFS was 13.2 (95% CI: 6.8-15.0) mo, 10.0 (95% CI: 2.4-18.6) mo, and 7.6 (95% CI: 2.8-Not reached) mo in pts aged ≥75, with severe renal impairment, and HR cytogenetics, respectively. Overall response and very good partial response rates were 51.8% and 26.5% in elderly pts, 68.0% and 48.0% in pts with severe renal impairment, and 32.5% and 25.0% in pts with HR cytogenetics. In the overall effectiveness population, ORR and VGPR were 46.3% and 27.9%.
28.9% of elderly, 25.0% of HR cytogenetics, and 30.8% of renal impaired pts had at least one AE. 1 elderly pt and 1 pt with HR cytogenetics had an AE leading to permanent discontinuation of Isa. The incidence of neutropenia was 8.3%, 0%, and 7.5% in elderly, renal impaired, and HR cytogenetics pts. Infections and infestations occurred in 3 pts in the overall safety population — 2 in elderly, 1 in renal impaired, and 0 in HR cytogenetics pts.
Conclusions: The effectiveness and safety profiles across elderly, renal impaired, and HR cytogenetics subgroups were similar to those in the overall effectiveness population. The results of this subgroup analyses continue to support Isa-Pd for treatment of RRMM across subgroups.
