Treatment of Newly Diagnosed Myeloma - Non-Transplant Eligible
Poster Session 1
P-110: Ixazomib maintenance in transplant-ineligible patients with newly diagnosed multiple myeloma: Final overall survival analysis from the TOURMALINE-MM4 study
Wednesday, September 27, 2023
1:30 PM - 2:30 PM EEST
.jpg)
Meletios A. Dimopoulos, MD
Professor and Chairman of the Department of Clinical Therapeutics
National and Kapodistrian University of Athens, United States
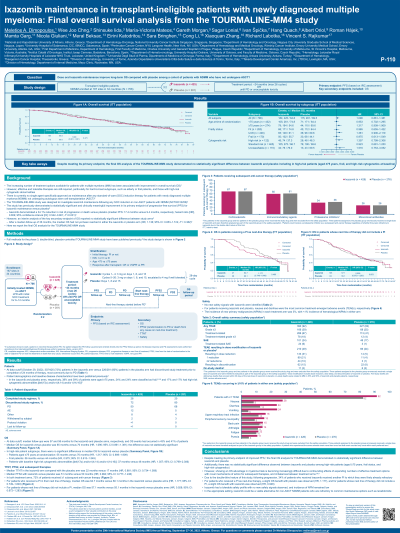
Introduction: The double-blind TOURMALINE-MM4 study (NCT02312258) included patients (pts) with newly diagnosed multiple myeloma (NDMM) who were ineligible for autologous stem cell transplantation (ASCT; Dimopoulos, J Clin Oncol 2020). The study previously demonstrated a statistically significant and clinically meaningful improvement in its primary endpoint of progression-free survival (PFS) for ixazomib (ixa) vs placebo (pbo) maintenance. An interim analysis showed no statistically significant difference in the key secondary endpoint of overall survival (OS; Dimopoulos, ASH 2021). We present the final OS analysis.
Methods: Full methods have been published previously (Dimopoulos, J Clin Oncol 2020). Eligible pts were randomized to receive single agent ixa (n=425) or pbo maintenance (n=281) for up to twenty-six 28-day cycles, or until progressive disease (PD) or unacceptable toxicity.
Results: At data cut (Oct 29, 2022 ), median follow-up for ixa vs pbo was 57 vs 58 months, OS events had occurred in 43 vs 41% of pts, and median OS was 65 vs 70 months (not statistically significant; hazard ratio [HR] 1.090; 95% confidence interval [CI] 0.861–1.381). There were no significant differences in median OS for ixa vs pbo among pts aged ≥75 years at randomization (55 vs 70 months; HR 1.317; 95% CI 0.909─1.909 ), frail pts (56 vs 44 months; HR 0.975; 95% CI 0.613─1.549 ), and pts with baseline high-risk cytogenetics [del(17p) and/or t(4;14) and/or t(14;16); 37 vs 48 months; HR 1.357; 95% CI 0.799─2.306 ]. Median PFS2 (PFS on next-line therapy) for ixa vs pbo was 51 vs 50 months (not significant; HR 0.984; 95% CI 0.777─1.246); median time to next therapy was 22 vs 17 months (not significant; HR 0.881; 95% CI 0.734–1.058 ). For ixa vs pbo, 72% of pts in each arm received ≥1 subsequent anti-cancer therapy, including: corticosteroids (67 vs 67%); immunomodulatory drugs (60 vs 61%); proteasome inhibitors (PI; 34 vs 36%); and monoclonal antibodies (26 vs 26%). The incidence of new primary malignancies (NPMs) in each treatment arm was 3%, with < 1% incidence of hematological NPMs in either arm; no new safety signals were identified.
Conclusions: The final OS analysis for TOURMALINE-MM4 showed no statistically significant difference between ixa and pbo, including among high-risk pts, despite the study meeting its primary endpoint. However, showing an OS advantage in myeloma trials is becoming increasingly difficult due to confounding effects of expanding numbers of effective treatment options with novel mechanisms of action for subsequent therapies, and imbalances in these therapies between treatment arms. Notably, due to the double-blind study design, following progression, 34% of pts who received ixa received another PI to which they were likely already refractory. Ixa had a tolerable safety profile and NPM incidence remained low. In the appropriate setting, ixa could be a viable alternative for non-ASCT NDMM pts who are refractory to common maintenance options such as lenalidomide.
Methods: Full methods have been published previously (Dimopoulos, J Clin Oncol 2020). Eligible pts were randomized to receive single agent ixa (n=425) or pbo maintenance (n=281) for up to twenty-six 28-day cycles, or until progressive disease (PD) or unacceptable toxicity.
Results: At data cut (Oct 29, 2022 ), median follow-up for ixa vs pbo was 57 vs 58 months, OS events had occurred in 43 vs 41% of pts, and median OS was 65 vs 70 months (not statistically significant; hazard ratio [HR] 1.090; 95% confidence interval [CI] 0.861–1.381). There were no significant differences in median OS for ixa vs pbo among pts aged ≥75 years at randomization (55 vs 70 months; HR 1.317; 95% CI 0.909─1.909 ), frail pts (56 vs 44 months; HR 0.975; 95% CI 0.613─1.549 ), and pts with baseline high-risk cytogenetics [del(17p) and/or t(4;14) and/or t(14;16); 37 vs 48 months; HR 1.357; 95% CI 0.799─2.306 ]. Median PFS2 (PFS on next-line therapy) for ixa vs pbo was 51 vs 50 months (not significant; HR 0.984; 95% CI 0.777─1.246); median time to next therapy was 22 vs 17 months (not significant; HR 0.881; 95% CI 0.734–1.058 ). For ixa vs pbo, 72% of pts in each arm received ≥1 subsequent anti-cancer therapy, including: corticosteroids (67 vs 67%); immunomodulatory drugs (60 vs 61%); proteasome inhibitors (PI; 34 vs 36%); and monoclonal antibodies (26 vs 26%). The incidence of new primary malignancies (NPMs) in each treatment arm was 3%, with < 1% incidence of hematological NPMs in either arm; no new safety signals were identified.
Conclusions: The final OS analysis for TOURMALINE-MM4 showed no statistically significant difference between ixa and pbo, including among high-risk pts, despite the study meeting its primary endpoint. However, showing an OS advantage in myeloma trials is becoming increasingly difficult due to confounding effects of expanding numbers of effective treatment options with novel mechanisms of action for subsequent therapies, and imbalances in these therapies between treatment arms. Notably, due to the double-blind study design, following progression, 34% of pts who received ixa received another PI to which they were likely already refractory. Ixa had a tolerable safety profile and NPM incidence remained low. In the appropriate setting, ixa could be a viable alternative for non-ASCT NDMM pts who are refractory to common maintenance options such as lenalidomide.
