Myeloma Novel Drug Targets and agents
Poster Session 2
P-184: Lenalidomide: Rash or no rash, that is the question
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST

Akshitha Devaraj, MBBS
Internal Medicine Trainee 1
Norfolk and Norrwich University Hospitals
St Albans, England, United Kingdom
Introduction: Lenalidomide is an immunomodulatory (IMID) drug used as a backbone in many myeloma therapy regimens. Its mechanism of action is complex exerting a pleiotropic anti-myeloma effect in vitro including immune-modulation, anti-angiogenic, anti-inflammatory and anti-proliferative effects. However, the relative in vivo contribution of each is poorly understood.
The toxicity profile of Lenalidomide is well known. It includes skin rash, pruritus, and photosensitivity. The mechanism by which lenalidomide may cause skin toxicity is not fully understood. However, studies suggest that lenalidomide can cause an immune-mediated reaction in the skin, particularly through T cell dysregulation. Lenalidomide is known to increase the production of Th1 cells, which are involved in the immune response. It is hypothesised that the increase in Th1 cells leads to an overactive immune response resulting in inflammation and tissue damage.
Recently we have observed a high incidence of skin toxicity in patients receiving lenalidomide. This may have an impact on treatment, compliance and potentially result in cessation of treatment.
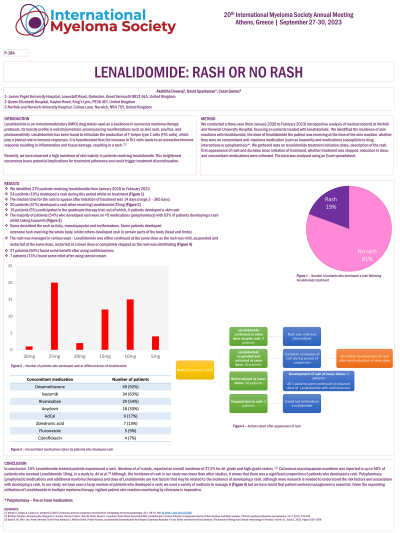
Methods: We reviewed the notes and collected data from the medical records of all patients who received lenalidomide over a 3-year period at Norfolk and Norwich University Hospital. We identified the incidence of skin reactions with lenalidomide, the dose of lenalidomide the at the time of the skin reaction, concomitant use of anti-myeloma medication (such as ixazomib) and other medications which could result in drug interactions or polypharmacy.
Results: Of the 279 patients receiving lenalidomide, 54 patients (19%) developed a rash during their treatment. The median time for the rash to appear after initiation of treatment was 14 days (range 3 days and 365 days). 15 patients (5%) participated in the quadruple therapy trial; out of which, 4 patients developed a skin rash. Furthermore, 3 patients (1%) participated in the triple therapy trial – interestingly, all 3 patients developed a rash.
Of the 54 patients who developed a rash, lenalidomide was stopped in 20 patients; the discontinuation of treatment resulted in complete resolution of the rash. Lenalidomide was reintroduced to 7 patients (13%) and was subsequently stopped in 4 patients. The dose was reduced to 15mg from 25mg in 3 patients – these patients were continued on 15mg with no further incidences of a rash. However, when lenalidomide was reintroduced at a lower dose (15mg and 10mg) for 2 patients, they developed rash and treatment was discontinued.
Conclusions: In conclusion, 19% of patients who received lenalidomide treatment developed a rash. A study by Nardone et al found that the overall incidence of all-grade and high-grade rash was 27.2%.[4] There was 100% resolution of symptoms when lenalidomide was stopped. With the increase in lenalidomide in multiple myeloma treatment, it is imperative that clinicians monitor their patients for skin reactions.
The toxicity profile of Lenalidomide is well known. It includes skin rash, pruritus, and photosensitivity. The mechanism by which lenalidomide may cause skin toxicity is not fully understood. However, studies suggest that lenalidomide can cause an immune-mediated reaction in the skin, particularly through T cell dysregulation. Lenalidomide is known to increase the production of Th1 cells, which are involved in the immune response. It is hypothesised that the increase in Th1 cells leads to an overactive immune response resulting in inflammation and tissue damage.
Recently we have observed a high incidence of skin toxicity in patients receiving lenalidomide. This may have an impact on treatment, compliance and potentially result in cessation of treatment.
Methods: We reviewed the notes and collected data from the medical records of all patients who received lenalidomide over a 3-year period at Norfolk and Norwich University Hospital. We identified the incidence of skin reactions with lenalidomide, the dose of lenalidomide the at the time of the skin reaction, concomitant use of anti-myeloma medication (such as ixazomib) and other medications which could result in drug interactions or polypharmacy.
Results: Of the 279 patients receiving lenalidomide, 54 patients (19%) developed a rash during their treatment. The median time for the rash to appear after initiation of treatment was 14 days (range 3 days and 365 days). 15 patients (5%) participated in the quadruple therapy trial; out of which, 4 patients developed a skin rash. Furthermore, 3 patients (1%) participated in the triple therapy trial – interestingly, all 3 patients developed a rash.
Of the 54 patients who developed a rash, lenalidomide was stopped in 20 patients; the discontinuation of treatment resulted in complete resolution of the rash. Lenalidomide was reintroduced to 7 patients (13%) and was subsequently stopped in 4 patients. The dose was reduced to 15mg from 25mg in 3 patients – these patients were continued on 15mg with no further incidences of a rash. However, when lenalidomide was reintroduced at a lower dose (15mg and 10mg) for 2 patients, they developed rash and treatment was discontinued.
Conclusions: In conclusion, 19% of patients who received lenalidomide treatment developed a rash. A study by Nardone et al found that the overall incidence of all-grade and high-grade rash was 27.2%.[4] There was 100% resolution of symptoms when lenalidomide was stopped. With the increase in lenalidomide in multiple myeloma treatment, it is imperative that clinicians monitor their patients for skin reactions.
