Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-296: LIGHTHOUSE: MELFLUFEN, DARATUMUMAB, AND DEXAMETHASONE VERSUS DARATUMUMAB IN RELAPSED/REFRACTORY MULTIPLE MYELOMA REFRACTORY TO AN IMID AND A PROTEASOME INHIBITOR OR WITH ≥3 PRIOR LINES OF THERAPY
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST

María-Victoria Mateos, MD, PhD
Professor
University Hospital of Salamanca/IBSAL/CIC/CIBERONC, Salamanca, Spain
Salamanca, Spain
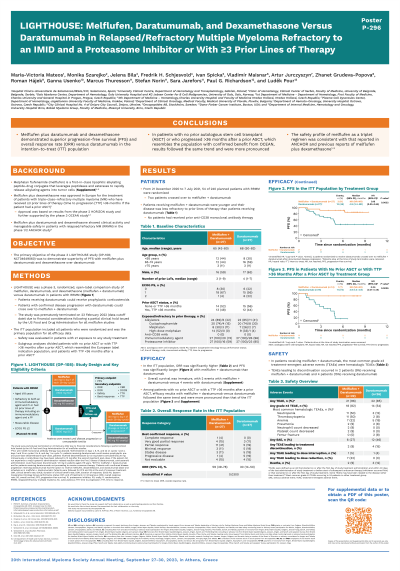
Introduction: Melphalan flufenamide (melflufen), a first-in-class peptide-drug conjugate (PDC), and dexamethasone (dex) is approved in Europe for use in patients (pts) with ≥3 prior lines of therapy (LoTs) and triple-class refractory RRMM (time to progression [TTP] >36 mo if pt had a prior autologous stem cell transplant [ASCT]). Results from the phase 2 HORIZON and phase 3 OCEAN studies supported the approval. Melflufen + daratumumab + dex (Dd) showed clinical activity and manageable safety in the phase 1/2 ANCHOR study (Ocio EM, et al. ASH 2020, abstract 417), and was further assessed in the phase 3 LIGHTHOUSE study (NCT04649060).
Methods: Pts with RRMM, refractory to an IMiD and a proteasome inhibitor (PI) or with ≥3 prior LoTs including an IMiD and a PI, were randomized (1:1) to 28-day cycles (C) of intravenous melflufen (30 mg on day 1 per cycle) + oral dex (40 mg weekly; 20 mg if aged ≥75 y) + subcutaneous Dara (1800 mg on days 1, 8, 15, and 22 in C1-2, day 1 and 15 in C3-6, and day 1 in C7+) or Dara monotherapy (regimen as in the melflufen arm) until disease progression or unacceptable toxicity. Prior anti-CD38 monoclonal antibody therapy was allowed, but no pts had received it. Pts with confirmed disease progression in the Dara arm could cross over to melflufen + Dd. Primary endpoint: progression-free survival (PFS). Key secondary endpoints: overall response rate (ORR) and safety. Financial considerations after a partial clinical hold issued by the FDA for all melflufen studies led to premature study closure (23 Feb 2022; data cutoff date).
Results: From 21 Dec 2020 to 7 Jul 2021, 54 of 240 planned pts were randomized (melflufen + Dd, n=27; Dara, n=27); 2 pts crossed over to melflufen + Dd. With melflufen + Dd vs Dara, median age was 65 y vs 68 y, 11 (41%) vs 13 (48%) had no prior ASCT, and 3 (11%) vs 2 (7%) had a TTP >36 mo after a prior ASCT, respectively. Median PFS was not reached (NR) with melflufen + Dd vs 4.9 mo with Dara (hazard ratio [HR], 0.18 [95% CI, 0.05-0.65]; P=0.0032). ORR was 59.3% with melflufen + Dd vs 29.6% with Dara (P=0.0300). OS was immature, with 2 events with melflufen + Dd vs 4 events with Dara (HR, 0.47 [95% CI, 0.09-2.57]; P=0.3721). Among pts with no prior ASCT or with a TTP >36 mo after a prior ASCT (melflufen + Dd, n=14; Dara, n=15), median PFS was NR with melflufen + Dd (1 event) vs 3.9 mo with Dara (11 events; HR, 0.06 [95% CI, 0.01-0.49]; P=0.0005), ORR was 64.3% vs 13.3% (P=0.0055), and 1 vs 4 OS events occurred (P=0.0369), respectively. With melflufen + Dd vs Dara, the most common grade ≥3 treatment-emergent adverse events were neutropenia (50% vs 12%), thrombocytopenia (50% vs 8%), and anemia (32% vs 19%), respectively.
Conclusions: Melflufen + Dd showed superior PFS and ORR vs Dara, including in pts with no prior ASCT or with a TTP >36 mo after a prior ASCT, which resembles the population with confirmed benefit from OCEAN. The safety profile of melflufen + Dd was consistent with previous reports of melflufen.
Methods: Pts with RRMM, refractory to an IMiD and a proteasome inhibitor (PI) or with ≥3 prior LoTs including an IMiD and a PI, were randomized (1:1) to 28-day cycles (C) of intravenous melflufen (30 mg on day 1 per cycle) + oral dex (40 mg weekly; 20 mg if aged ≥75 y) + subcutaneous Dara (1800 mg on days 1, 8, 15, and 22 in C1-2, day 1 and 15 in C3-6, and day 1 in C7+) or Dara monotherapy (regimen as in the melflufen arm) until disease progression or unacceptable toxicity. Prior anti-CD38 monoclonal antibody therapy was allowed, but no pts had received it. Pts with confirmed disease progression in the Dara arm could cross over to melflufen + Dd. Primary endpoint: progression-free survival (PFS). Key secondary endpoints: overall response rate (ORR) and safety. Financial considerations after a partial clinical hold issued by the FDA for all melflufen studies led to premature study closure (23 Feb 2022; data cutoff date).
Results: From 21 Dec 2020 to 7 Jul 2021, 54 of 240 planned pts were randomized (melflufen + Dd, n=27; Dara, n=27); 2 pts crossed over to melflufen + Dd. With melflufen + Dd vs Dara, median age was 65 y vs 68 y, 11 (41%) vs 13 (48%) had no prior ASCT, and 3 (11%) vs 2 (7%) had a TTP >36 mo after a prior ASCT, respectively. Median PFS was not reached (NR) with melflufen + Dd vs 4.9 mo with Dara (hazard ratio [HR], 0.18 [95% CI, 0.05-0.65]; P=0.0032). ORR was 59.3% with melflufen + Dd vs 29.6% with Dara (P=0.0300). OS was immature, with 2 events with melflufen + Dd vs 4 events with Dara (HR, 0.47 [95% CI, 0.09-2.57]; P=0.3721). Among pts with no prior ASCT or with a TTP >36 mo after a prior ASCT (melflufen + Dd, n=14; Dara, n=15), median PFS was NR with melflufen + Dd (1 event) vs 3.9 mo with Dara (11 events; HR, 0.06 [95% CI, 0.01-0.49]; P=0.0005), ORR was 64.3% vs 13.3% (P=0.0055), and 1 vs 4 OS events occurred (P=0.0369), respectively. With melflufen + Dd vs Dara, the most common grade ≥3 treatment-emergent adverse events were neutropenia (50% vs 12%), thrombocytopenia (50% vs 8%), and anemia (32% vs 19%), respectively.
Conclusions: Melflufen + Dd showed superior PFS and ORR vs Dara, including in pts with no prior ASCT or with a TTP >36 mo after a prior ASCT, which resembles the population with confirmed benefit from OCEAN. The safety profile of melflufen + Dd was consistent with previous reports of melflufen.
