Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-264: A Phase 1b Study of Isatuximab and Bendamustine for Triple-Class Refractory Multiple Myeloma
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST

Scott R. Goldsmith, MD (he/him/his)
Hematologist
City Of Hope National Medical Center, Duarte, CA, USA, California, United States
Introduction: Triple-class refractory MM is associated with poor outcomes. Bendamustine (Benda) has is an active cytotoxic chemotherapy regimen for MM that is well-tolerated with outpatient administration. Isatuximab (Isa) induces caspase-dependent cytotoxicity similar to rituximab. We hypothesized that Isa may synergize with Benda in patients with triple-class refractory disease.
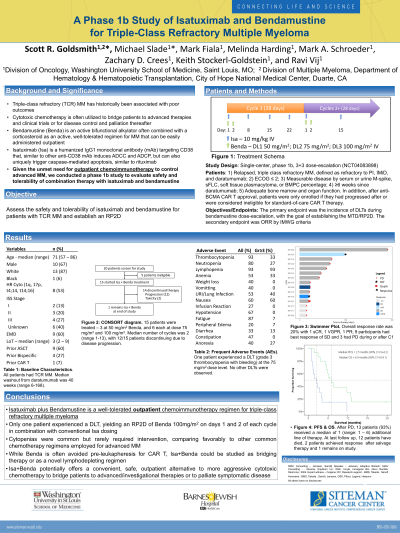
Methods: We conducted a single-center, phase 1b dose-escalation study to assess the safety, tolerability, and RP2D/MTD of Benda in combination with Isa in patient with triple-class refractory multiple myeloma, defined as treatment with proteasome inhibitor, an immunomodulatory drug, and daratumumab in combination or as single-agents and progression within 60 days of last dose. The study was approved by the local IRB and registered with clinicaltrials.gov (NCT04083898).
Patients were enrolled according to a 3+3 dose-escalation design. Isa was administered as 10 mg/kg IV on days 1, 8, 15, and 22 of cycle 1, and days 1 and 15 thereafter. Benda dose levels included: 50, 75, and 100 mg/m2 administered on days 1 and 2 of each cycle. Patients received methylprednisolone with each dose of Isa, and prednisone on days 2-4. After approval of standard-of-care CAR T therapy, patients were only enrolled if they had progressed after or were considered ineligible for CAR T. Adverse events were grade by CTCAE v 5.0. DLTs definitions adhered to standards for MM clinical trials.
Results: 15 patients were treated; 3 at 50 Benda, and 6 each at dose 75 and 100. The median age was 71 (56-85) and 10 were male. 8 had high-risk cytogenetics and 9 had extramedullary disease. The median prior lines of MM treatment was 3 (range 2-9) and 60% had underwent ASCT. The median time post-daratumumab was 40 weeks (range 6-168).
Cytopenias were common but rarely required intervention. There was only 1 DLT, at 50 benda (G3 thrombocytopenia with bleeding). 7 patients had infectious complications. The median number of cycles administered was 2 (range 1-13); at the time of abstract 2 patients are receiving treatment, both with bulky EMD and objective responses. There was 1 CR, 1 VGPR, 1 PR, and 9 SD.
Conclusions: Isa + Benda is a safe combination and the MTD was not reached. RP2D is 100mg/m2 of Benda on days 1 and 2 with conventional Isa dosing. Despite advanced disease with daratumumab-refractoriness, patients had notable disease control, including objective responses at the RP2D in patients with bulky EMD, a difficult subgroup. Unlike other cytoreductive chemotherapy for MM, this regimen allows for outpatient administration. Bendamustine may affect engineering and efficacy of cellular therapies, and is generally avoided pre-leukapheresis. However, Isa-Benda may serve as a reasonable bridging therapy that allows for disease control while reducing risk of severe cytopenias. Recent experience with Benda as a lymphodepleting agent has suggested comparable outcomes. Consequently, Isa-Benda as a novel MM lymphodepleting combination may warrant prospective study.
Methods: We conducted a single-center, phase 1b dose-escalation study to assess the safety, tolerability, and RP2D/MTD of Benda in combination with Isa in patient with triple-class refractory multiple myeloma, defined as treatment with proteasome inhibitor, an immunomodulatory drug, and daratumumab in combination or as single-agents and progression within 60 days of last dose. The study was approved by the local IRB and registered with clinicaltrials.gov (NCT04083898).
Patients were enrolled according to a 3+3 dose-escalation design. Isa was administered as 10 mg/kg IV on days 1, 8, 15, and 22 of cycle 1, and days 1 and 15 thereafter. Benda dose levels included: 50, 75, and 100 mg/m2 administered on days 1 and 2 of each cycle. Patients received methylprednisolone with each dose of Isa, and prednisone on days 2-4. After approval of standard-of-care CAR T therapy, patients were only enrolled if they had progressed after or were considered ineligible for CAR T. Adverse events were grade by CTCAE v 5.0. DLTs definitions adhered to standards for MM clinical trials.
Results: 15 patients were treated; 3 at 50 Benda, and 6 each at dose 75 and 100. The median age was 71 (56-85) and 10 were male. 8 had high-risk cytogenetics and 9 had extramedullary disease. The median prior lines of MM treatment was 3 (range 2-9) and 60% had underwent ASCT. The median time post-daratumumab was 40 weeks (range 6-168).
Cytopenias were common but rarely required intervention. There was only 1 DLT, at 50 benda (G3 thrombocytopenia with bleeding). 7 patients had infectious complications. The median number of cycles administered was 2 (range 1-13); at the time of abstract 2 patients are receiving treatment, both with bulky EMD and objective responses. There was 1 CR, 1 VGPR, 1 PR, and 9 SD.
Conclusions: Isa + Benda is a safe combination and the MTD was not reached. RP2D is 100mg/m2 of Benda on days 1 and 2 with conventional Isa dosing. Despite advanced disease with daratumumab-refractoriness, patients had notable disease control, including objective responses at the RP2D in patients with bulky EMD, a difficult subgroup. Unlike other cytoreductive chemotherapy for MM, this regimen allows for outpatient administration. Bendamustine may affect engineering and efficacy of cellular therapies, and is generally avoided pre-leukapheresis. However, Isa-Benda may serve as a reasonable bridging therapy that allows for disease control while reducing risk of severe cytopenias. Recent experience with Benda as a lymphodepleting agent has suggested comparable outcomes. Consequently, Isa-Benda as a novel MM lymphodepleting combination may warrant prospective study.
