Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-290: Updated long-term follow-up results of a phase 1b/2 study (FUMANBA-1) in patients with relapsed/refractory multiple myeloma (RRMM) treated with Equecabtagene Autoleucel
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST

Chunrui Li, MD
Prof.
Department of Hematology, Tongji Hospital of Tongji Medical College, Huazhong University of Science and Technology
Wuhan, Hubei, China (People's Republic)
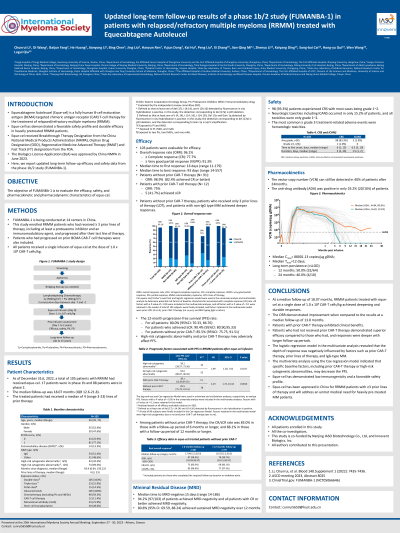
Introduction: Equecabtagene Autoleucel (Eque-cel) is a fully human B-cell maturation antigen (BCMA) targeted chimeric antigen receptor (CAR) T-cell therapy for relapsed/refractory multiple myeloma (RRMM). A phase 1b/2 study (FUMANBA-1) was conducted for Eque-cel in RRMM patients (NCT05066646). Here, we report the results of the FUMANBA-1 trial, which was conducted at 14 sites in China and had a median follow-up duration of 18.07 months (range: 0.4, 30.3).
Methods: Participants were RRMM patients who had received at least three prior lines of therapy (with at least one proteasome inhibitor and one immunomodulator) and whose disease had progressed after the last line of therapy. Patients with prior BCMA CAR -T therapy were also included. On three consecutive days of lymphodepletion (500mg/m2 cyclophosphamide and 30mg/m2 fludarabine), patients received a single infusion of Eque-cel at a dose of 1×10^6 cells/kg.
Results: As of December 31, 2022, 105 patients received Eque-cel with a median of 4 lines of prior therapy (range 3-23). 32.4% of patients had high-risk cytogenetic abnormalities (defined as at least one of del (17), t (4:14) and t (14:16) is positive), 13.3% had extramedullary disease (EMD), 11.4% had received prior BCMA CAR-T therapy, and 52.4% belonged to IgG-type MM.
Of the 103 patients whose efficacy could be evaluated, 96.1% achieved a response, 77.7% achieved a complete response (CR) or a stringent CR. The 12-month PFS rate was 80.0% (95% CI: 70.33, 86.76).
Patients without prior CAR-T therapy, patients who had already received three lines of treatment, and patients who were not IgG MM, achieved deeper responses, and the sCR/ CR rates were 82.4%, 96.3%, and 91.8%, respectively. Patients without high-risk cytogenetic abnormalities and without prior CAR-T therapy had better PFS rate, and 12-m PFS rates were 92.0% (95% CI: 80.07, 96.92) and 85.5% (95% CI: 75.75, 91.51), respectively.
Ninety-seven of 103 (94.2%) evaluable patients achieved MRD-negativity, including all ≥ CR patients. 90.0% of patients achieved ≥CR were persistently MRD-negative for ≥12 months. CRS occurred in 93.3% (98/105) of patients, and only one was ≥ grade 3. The median time to onset was six days (range: 1-13), and the median duration was 5 days (range: 2-30). ICANS occurred in 2 patients who had either grade 1 or 2. Eque-cel expansion in peripheral blood peaked at 88001.13 copies/μg gDNA, and the median time to peak level was 12 days post-infusion. CAR Transgenes were still detectable in 50% (32/64) of patients 12 months and in 40% (4/10) of patients 24 months after infusion. Anti-CAR antibodies developed in only 20 (19.2%) patients after infusion.
Conclusions: A profound and durable response can be achieved in RRMM patients treated with Eque-cel with a median follow-up of 18.07 months. Factors like prior CAR-T therapy, more prior lines of therapy and IgG-type MM could adversely impact the depth of response, and factors like prior CAR-T therapy or high-risk cytogenetic abnormalities might also reduce the PFS.
Methods: Participants were RRMM patients who had received at least three prior lines of therapy (with at least one proteasome inhibitor and one immunomodulator) and whose disease had progressed after the last line of therapy. Patients with prior BCMA CAR -T therapy were also included. On three consecutive days of lymphodepletion (500mg/m2 cyclophosphamide and 30mg/m2 fludarabine), patients received a single infusion of Eque-cel at a dose of 1×10^6 cells/kg.
Results: As of December 31, 2022, 105 patients received Eque-cel with a median of 4 lines of prior therapy (range 3-23). 32.4% of patients had high-risk cytogenetic abnormalities (defined as at least one of del (17), t (4:14) and t (14:16) is positive), 13.3% had extramedullary disease (EMD), 11.4% had received prior BCMA CAR-T therapy, and 52.4% belonged to IgG-type MM.
Of the 103 patients whose efficacy could be evaluated, 96.1% achieved a response, 77.7% achieved a complete response (CR) or a stringent CR. The 12-month PFS rate was 80.0% (95% CI: 70.33, 86.76).
Patients without prior CAR-T therapy, patients who had already received three lines of treatment, and patients who were not IgG MM, achieved deeper responses, and the sCR/ CR rates were 82.4%, 96.3%, and 91.8%, respectively. Patients without high-risk cytogenetic abnormalities and without prior CAR-T therapy had better PFS rate, and 12-m PFS rates were 92.0% (95% CI: 80.07, 96.92) and 85.5% (95% CI: 75.75, 91.51), respectively.
Ninety-seven of 103 (94.2%) evaluable patients achieved MRD-negativity, including all ≥ CR patients. 90.0% of patients achieved ≥CR were persistently MRD-negative for ≥12 months. CRS occurred in 93.3% (98/105) of patients, and only one was ≥ grade 3. The median time to onset was six days (range: 1-13), and the median duration was 5 days (range: 2-30). ICANS occurred in 2 patients who had either grade 1 or 2. Eque-cel expansion in peripheral blood peaked at 88001.13 copies/μg gDNA, and the median time to peak level was 12 days post-infusion. CAR Transgenes were still detectable in 50% (32/64) of patients 12 months and in 40% (4/10) of patients 24 months after infusion. Anti-CAR antibodies developed in only 20 (19.2%) patients after infusion.
Conclusions: A profound and durable response can be achieved in RRMM patients treated with Eque-cel with a median follow-up of 18.07 months. Factors like prior CAR-T therapy, more prior lines of therapy and IgG-type MM could adversely impact the depth of response, and factors like prior CAR-T therapy or high-risk cytogenetic abnormalities might also reduce the PFS.
