MRD Assessment and role in Myeloma
Poster Session 1
P-084: Use of Peripheral Blood for MRD Assessment During Maintenance Therapy: UTSW Experience
Wednesday, September 27, 2023
1:30 PM - 2:30 PM EEST

Aishwarya Sannareddy, MBBS (she/her/hers)
Senior Researcher
UT Southwestern Medical Center
Dallas, Texas, United States
Introduction: Over the years, the treatment modalities for patients diagnosed with Multiple Myeloma (MM) have improved and evolved. Lasting responses and increase in survival outcomes to newer therapies have led to development of advanced tools used to assess the disease pattern. Minimal residual disease (MRD) test is one such tool which detects cancer cells in remission and identifies increasing numbers of tumor cells. This increase in the number of tumor cells may lead to relapse, with a potential to inform clinical decisions on therapy intensification or de-escalation. Bone marrow (BM) biopsies are ideal for MRD assessment in MM patients. There is interest in peripheral blood (PB) use for assessment, which is less invasive, allowing frequent monitoring. In our real-world data set, we studied PB MRD use in patients who were MRD tested by the clonoSEQ® assay (Adaptive Biotechnologies).
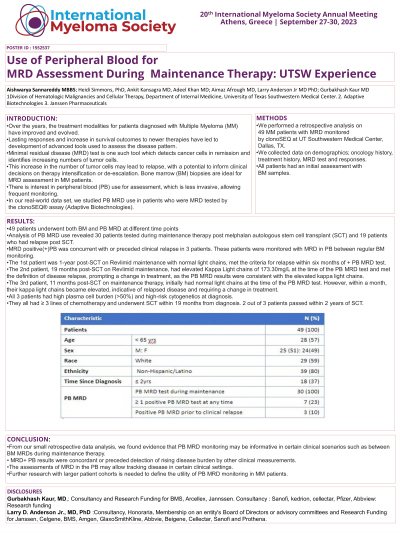
Methods: We performed a retrospective analysis on 49 MM patients with MRD monitored by clonoSEQ at UT Southwestern Medical Center, Dallas, TX. We collected data on demographics; oncology history, treatment history, MRD test and responses. All patients had a initial assessment with BM samples.
Results: 49 patients underwent both BM and PB MRD at different time points. Analysis of PB MRD use revealed 30 patients tested during maintenance therapy post melphalan autologous stem cell transplant (SCT) and 19 patients who had relapse post SCT. MRD positive(+)PB was concurrent with or preceded clinical relapse in 3 patients. These patients were monitored with MRD in PB between regular BM monitoring. The 1st patient was 1 year post-SCT on Revlimid maintenance with normal light chains, met the criteria for relapse within six months of + PB MRD test. The 2nd patient, 19 months post-SCT on Revlimid maintenance, had elevated Kappa Light chains of 173.30mg/L at the time of the PB MRD test and met the definition of disease relapse, prompting a change in treatment, as the PB MRD results were consistent with the elevated kappa light chains. The 3rd patient, 11 months post-SCT on maintenance therapy, initially had normal light chains at the time of the PB MRD test. However, within a month, their kappa light chains became elevated, indicative of relapsed disease and requiring a change in treatment. All 3 patients had high plasma cell burden (>50%) and high-risk cytogenetics at diagnosis. They all had ≥ 3 lines of chemotherapy and underwent SCT within 19 months from diagnosis. 2 out of 3 patients passed within 2 years of SCT.
Conclusions: From our small retrospective data analysis, we found evidence that PB MRD monitoring may be informative in certain clinical scenarios such as between BM MRDs during maintenance therapy. MRD+ PB results were concordant or preceded detection of rising disease burden by other clinical measurements. The assessments of MRD in the PB may allow tracking disease in certain clinical settings. Further research with larger patient cohorts is needed to define the utility of PB MRD monitoring in MM patients.
Methods: We performed a retrospective analysis on 49 MM patients with MRD monitored by clonoSEQ at UT Southwestern Medical Center, Dallas, TX. We collected data on demographics; oncology history, treatment history, MRD test and responses. All patients had a initial assessment with BM samples.
Results: 49 patients underwent both BM and PB MRD at different time points. Analysis of PB MRD use revealed 30 patients tested during maintenance therapy post melphalan autologous stem cell transplant (SCT) and 19 patients who had relapse post SCT. MRD positive(+)PB was concurrent with or preceded clinical relapse in 3 patients. These patients were monitored with MRD in PB between regular BM monitoring. The 1st patient was 1 year post-SCT on Revlimid maintenance with normal light chains, met the criteria for relapse within six months of + PB MRD test. The 2nd patient, 19 months post-SCT on Revlimid maintenance, had elevated Kappa Light chains of 173.30mg/L at the time of the PB MRD test and met the definition of disease relapse, prompting a change in treatment, as the PB MRD results were consistent with the elevated kappa light chains. The 3rd patient, 11 months post-SCT on maintenance therapy, initially had normal light chains at the time of the PB MRD test. However, within a month, their kappa light chains became elevated, indicative of relapsed disease and requiring a change in treatment. All 3 patients had high plasma cell burden (>50%) and high-risk cytogenetics at diagnosis. They all had ≥ 3 lines of chemotherapy and underwent SCT within 19 months from diagnosis. 2 out of 3 patients passed within 2 years of SCT.
Conclusions: From our small retrospective data analysis, we found evidence that PB MRD monitoring may be informative in certain clinical scenarios such as between BM MRDs during maintenance therapy. MRD+ PB results were concordant or preceded detection of rising disease burden by other clinical measurements. The assessments of MRD in the PB may allow tracking disease in certain clinical settings. Further research with larger patient cohorts is needed to define the utility of PB MRD monitoring in MM patients.
