Treatment of Relapsed/Refractory Myeloma
Poster Session 2
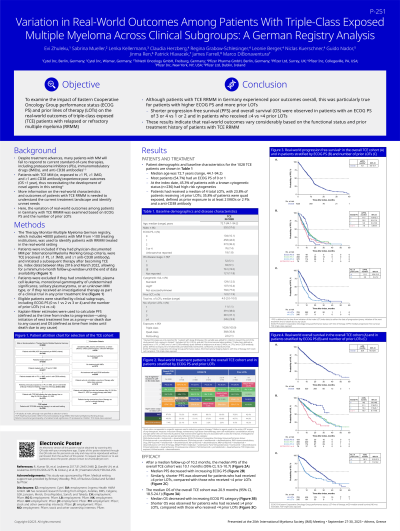
P-251: VARIATION IN REAL-WORLD OUTCOMES AMONG PATIENTS WITH TRIPLE-CLASS EXPOSED MULTIPLE MYELOMA ACROSS CLINICAL SUBGROUPS: A GERMAN REGISTRY ANALYSIS
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST

Marco DiBonaventura, PhD (he/him/his)
Senior Director, Value & Evidence Team Lead, Hematology & Biosimilars
Pfizer Inc
New York, New York, United States
Introduction: Multiple myeloma (MM) patients who have been exposed to at least 1 proteasome inhibitor, 1 immunomodulatory drug, and 1 anti-CD38 antibody (ie, triple-class exposed [TCE]) experience poor outcomes. This analysis examined the variation of real-world TCE outcomes as a function of ECOG performance status and number of prior lines of therapy (LOTs).
Methods: Data from the Therapy Monitor-Multiple Myeloma (TM-MM) Germany registry were used, which includes approximately 8,000 patients (pts) with MM from a representative sample of >100 treating institutions. Pts were included in the analysis if they had physician-documented MM per IMWG diagnosis criteria, were TCE, and initiated a subsequent therapy after becoming TCE (ie, index date) between May 2016 and March 2022, allowing for a minimum 6-month follow-up window until the end of data availability (September 2022). Pts with smoldering disease or active plasma cell leukemia were excluded, as were pts who had received an investigational treatment line as part of a clinical trial. Eligible pts were stratified by clinical subgroups including ECOG score (0 vs 1 vs 2 vs 3-4) and the number of prior LOTs ( < 4 vs ≥4). Using Kaplan-Meier estimates, progression-free survival (PFS), defined as time from index to progression (with initiation of the next treatment line as a proxy) or death due to any cause and overall survival (OS), defined as time from index until death due to any cause, were calculated.
Results: A total of N=1,028 TCE pts were included in the analyses (median age=72.7 years [range: 44.1 to 94.2], 57.6% male. At the index date, 10.4% were high-risk based on the presence of t(4:14), t(14:16), and/or del17p (ie, genomic features based on R-ISS; though 77.0% of pts had unknown/unassessed cytogenetic risk); 10.1%, 44.6%, and 36.2% had ECOG scores of 0, 1, and 2, with the remaining 7.4% having an ECOG of 3 or 4. Pts had received a median of 3 prior LOTs with 35.8% being quad-exposed. Median PFS (mPFS) decreased with increasing ECOG score category: ECOG 0=11.7 months (95% confidence interval: 11.3 months, 12.1 months); ECOG 1=10.2 months (9.0, 11.4); ECOG 2=9.6 months (8.0, 10.6); and ECOG 3/4=7.8 months (5.9, 9.9). Similarly, shorter mPFS (5.8 months [5.0, 7.2] vs 11.0 months [10.4, 11.6] was observed for prior LOT≥4 and < 4, respectively). mOS also decreased with increasing ECOG score category: ECOG 0=not estimable (NE) (30.0, NE); ECOG 1=21.1 months (17.8, 27.0); ECOG 2=19.4 months (17.8, 24.7); ECOG 3/4=10.7 months (9.1, 14.6). Shorter mOS (8.7 months [7.0, 12.2] vs 24.3 months [21.3, 27.5]) was also observed for pts with ≥4 prior LOTs.
Conclusions: Although TCE MM pts in Germany experience poor outcomes overall, this was particularly true for pts with higher ECOG scores and more prior LOTs. The results highlight the necessity to use all available therapeutic options in early lines of therapy.
Methods: Data from the Therapy Monitor-Multiple Myeloma (TM-MM) Germany registry were used, which includes approximately 8,000 patients (pts) with MM from a representative sample of >100 treating institutions. Pts were included in the analysis if they had physician-documented MM per IMWG diagnosis criteria, were TCE, and initiated a subsequent therapy after becoming TCE (ie, index date) between May 2016 and March 2022, allowing for a minimum 6-month follow-up window until the end of data availability (September 2022). Pts with smoldering disease or active plasma cell leukemia were excluded, as were pts who had received an investigational treatment line as part of a clinical trial. Eligible pts were stratified by clinical subgroups including ECOG score (0 vs 1 vs 2 vs 3-4) and the number of prior LOTs ( < 4 vs ≥4). Using Kaplan-Meier estimates, progression-free survival (PFS), defined as time from index to progression (with initiation of the next treatment line as a proxy) or death due to any cause and overall survival (OS), defined as time from index until death due to any cause, were calculated.
Results: A total of N=1,028 TCE pts were included in the analyses (median age=72.7 years [range: 44.1 to 94.2], 57.6% male. At the index date, 10.4% were high-risk based on the presence of t(4:14), t(14:16), and/or del17p (ie, genomic features based on R-ISS; though 77.0% of pts had unknown/unassessed cytogenetic risk); 10.1%, 44.6%, and 36.2% had ECOG scores of 0, 1, and 2, with the remaining 7.4% having an ECOG of 3 or 4. Pts had received a median of 3 prior LOTs with 35.8% being quad-exposed. Median PFS (mPFS) decreased with increasing ECOG score category: ECOG 0=11.7 months (95% confidence interval: 11.3 months, 12.1 months); ECOG 1=10.2 months (9.0, 11.4); ECOG 2=9.6 months (8.0, 10.6); and ECOG 3/4=7.8 months (5.9, 9.9). Similarly, shorter mPFS (5.8 months [5.0, 7.2] vs 11.0 months [10.4, 11.6] was observed for prior LOT≥4 and < 4, respectively). mOS also decreased with increasing ECOG score category: ECOG 0=not estimable (NE) (30.0, NE); ECOG 1=21.1 months (17.8, 27.0); ECOG 2=19.4 months (17.8, 24.7); ECOG 3/4=10.7 months (9.1, 14.6). Shorter mOS (8.7 months [7.0, 12.2] vs 24.3 months [21.3, 27.5]) was also observed for pts with ≥4 prior LOTs.
Conclusions: Although TCE MM pts in Germany experience poor outcomes overall, this was particularly true for pts with higher ECOG scores and more prior LOTs. The results highlight the necessity to use all available therapeutic options in early lines of therapy.
