Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-309: ZnDDC, a novel CELMoD-like agent binding to DDB1-CRBN complex demonstrates significant synergism with BTZ and IMiDs and overcomes IMiDs resistance in myeloma cell lines and primary samples
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST

Gowtham Rajendran (he/him/his)
PhD student
University of Wolverhampton
wolverhampton, England, United Kingdom
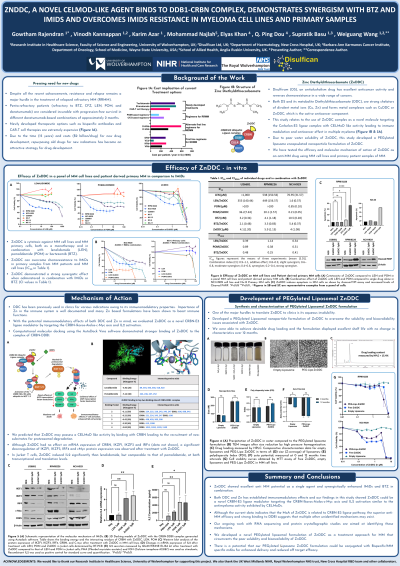
Introduction: Although immunomodulatory imide drugs (IMiDs), also called CRBN E3 ligase modulatory drugs (CELMoDs), e.g., lenalidamide (LEN), pomalidomide (POM) and proteasome inhibitor [bortezomib (BTZ)] improved the survival rate of multiple myeloma (MM), all MM patients are relapsed due to drug resistance. Therefore, development of new IMiDs is of clinical urgency. Due to the time (15 years) and costs (£1.5 billion/drug) for new drug development, repositioning of old drugs for new indications is an emerging economical strategy. Disulfiram (DS), an anti-alcoholism drug used in clinic for over 60 years, demonstrates excellent specific anticancer activity with no/low toxicity to normal tissues. DS chelates copper (Cu) and zinc (Zn) to form copper-diethyldithiocarbamate (CuDDC) and zinc-diethyldithiocarbamate (ZnDDC) which are the active anticancer compounds. Although the anticancer activity of DS has been known for more than three decades, its application in cancer clinic has been limited by its very short half-life in the bloodstream ( < 4 min). In the recent years, we developed long half-life injectable DS showing strong anticancer efficacy in numerous cancer animal models. In this study, we developed a novel PEGylated liposome encapsulated ZnDDC (PEG-Lipo/ZnDDC) which shows stronger immunomodulatory and anti-MM effect than currently available IMiDs (LEN and POM) and reverses resistance, and synergistically enhances the anti-MM activity of IMiDs and BTZ.
Methods: MTT assay, RT-PCR, Western blot, Fluorescence imaging, Flow cytometry, Magnetic bead primary MM cell isolation and culture, HPLC, isobologram analysis, Nano formulation techniques, computer docking and modelling.
Results: We successfully developed PEG-Lipo/ZnDDC with satisfied drug loading content and controlled releasing. ZnDDC showed strong cytotoxicity in MM cell lines and patient-derived MM cells (IC50s: 5-10µM) in normoxic and hypoxic conditions. ZnDDC synergistically enhanced the cytotoxicity of IMiDs and BTZ and reversed their chemoresistance in normoxic and hypoxic conditions. Although ZnDDC had no effect on mRNA expression of cereblon (CRBN), IKZF1, IKZF3 and IRF4, a significant downregulation of IKZF1, IKZF3, IRF4 and cMyc proteins was observed after treating the MM cell lines with sub-cytotoxic concentrations of ZnDDC (2-5 µM). After exposure to low concentration of ZnDDC, levels of both IL-2 mRNA and protein were significantly boosted in T lymphocytes. Computer modelling through molecular docking using the AutoDock Vina software demonstrated a very strong binding of ZnDDC to the DDB1-CRBN complex, similar to that of LEN and POM. ZnDDC also reversed hypoxia-induced IMiDs and BTZ resistance in tested MM cell lines.
Conclusions: ZnDDC demonstrates CELMoD like property with synergistic effect when used in combination with clinically available IMiDs and BTZ; The effect of ZnDDC is potentially CRL4CRBN-IKZF1/3-IRF4 pathway dependent; Further study is ongoing which could translate this work into MM clinic in a fast track.
Methods: MTT assay, RT-PCR, Western blot, Fluorescence imaging, Flow cytometry, Magnetic bead primary MM cell isolation and culture, HPLC, isobologram analysis, Nano formulation techniques, computer docking and modelling.
Results: We successfully developed PEG-Lipo/ZnDDC with satisfied drug loading content and controlled releasing. ZnDDC showed strong cytotoxicity in MM cell lines and patient-derived MM cells (IC50s: 5-10µM) in normoxic and hypoxic conditions. ZnDDC synergistically enhanced the cytotoxicity of IMiDs and BTZ and reversed their chemoresistance in normoxic and hypoxic conditions. Although ZnDDC had no effect on mRNA expression of cereblon (CRBN), IKZF1, IKZF3 and IRF4, a significant downregulation of IKZF1, IKZF3, IRF4 and cMyc proteins was observed after treating the MM cell lines with sub-cytotoxic concentrations of ZnDDC (2-5 µM). After exposure to low concentration of ZnDDC, levels of both IL-2 mRNA and protein were significantly boosted in T lymphocytes. Computer modelling through molecular docking using the AutoDock Vina software demonstrated a very strong binding of ZnDDC to the DDB1-CRBN complex, similar to that of LEN and POM. ZnDDC also reversed hypoxia-induced IMiDs and BTZ resistance in tested MM cell lines.
Conclusions: ZnDDC demonstrates CELMoD like property with synergistic effect when used in combination with clinically available IMiDs and BTZ; The effect of ZnDDC is potentially CRL4CRBN-IKZF1/3-IRF4 pathway dependent; Further study is ongoing which could translate this work into MM clinic in a fast track.
