Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-227: Safety and clinical activity of ruxolitinib combined with carfilzomib and dexamethasone for patients with carfilzomib-refractory multiple myeloma:Rresults from a phase 1 clinical trial.
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST

Shebli Atrash, MD
hematology & oncology
Levine Cancer Institute
Charlotte, North Carolina, United States
Introduction: Ruxolitinib (Rux) is a selective Janus kinase 1/2 inhibitor approved for the treatment of patients with polycythemia vera, myelofibrosis, and refractory Graft-versus-host disease. Preclinical studies showed Rux could block the expression of MUC1 and inhibit the STAT pathway leading to modulation of IL-6-mediated myeloma cell refractoriness and reverse checkpoint inhibition by downregulating PD-L1 and PD-L2 expression on both myeloma and stromal cells (Chen et al. 2019). We conducted a phase 1 trial to determine the safety and preliminary efficacy of Rux in combination with carfilzomib for patients with carfilzomib-refractory, relapsed/refractory multiple myeloma.
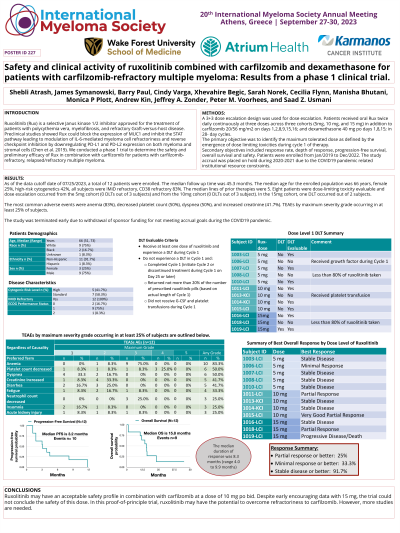
Methods: A 3+3 dose escalation design was used for dose escalation. Patients received oral Rux twice daily continuously at three doses across three cohorts (5mg, 10 mg, and 15 mg) in addition to carfilzomib 20/56 mg/m2 on days 1,2,8,9,15,16; and dexamethasone 40 mg po days 1,8,15; in 28-day cycles. The primary objective was to identify the maximum tolerated dose as defined by the emergence of dose limiting toxicities during cycle 1 of therapy. Secondary objectives included response rate, depth of response, progression-free survival, overall survival and safety. Patients were enrolled from Jan/2019 to Dec/2022. The study accrual was placed on hold during 2020-2021 due to the COVID19 pandemic related institutional resource constraints.
Results: As of the data cutoff date of March 6, 2023, a total of 12 patients were enrolled. The median follow up time was 42.2 months. The median age for the enrolled population was 66 years, female 25%, high-risk cytogenetics 42%, all subjects were IMiD refractory, CD38 refractory 83%. The median lines of prior therapies were 5. Eight patients were dose-limiting toxicity evaluable and dose escalation occurred from the 5mg cohort (0 DLTs out of 3 subjects) and from the 10mg cohort (0 DLTs out of 3 subject). In the 15mg cohort, one DLT occurred out of 2 subjects.
The most common adverse events were anemia (83%), decreased platelet count (50%), dyspnea (50%), and increased creatinine (41.7%). TEAEs by maximum severity grade occurring in at least 25% of subjects are shown in Table 1.
The best response observed in this trial was a VGPR in one subject. The overall response rate was 25%. The median progression-free survival time was 3.2 months, and the overall survival time was 15.8 months.
The study was terminated early due to withdrawal of sponsor funding for not meeting accrual goals during the COVID19 pandemic.
Conclusions: Ruxolitinib may have an acceptable safety profile in combination with carfilzomib at a dose of 10 mg po bid. Despite early encouraging data with 15 mg, the trial could not conclude the safety of this dose. In this proof-of-principle trial, ruxolitinib may have the potential to overcome refractoriness to carfilzomib. However, more studies are needed.
Methods: A 3+3 dose escalation design was used for dose escalation. Patients received oral Rux twice daily continuously at three doses across three cohorts (5mg, 10 mg, and 15 mg) in addition to carfilzomib 20/56 mg/m2 on days 1,2,8,9,15,16; and dexamethasone 40 mg po days 1,8,15; in 28-day cycles. The primary objective was to identify the maximum tolerated dose as defined by the emergence of dose limiting toxicities during cycle 1 of therapy. Secondary objectives included response rate, depth of response, progression-free survival, overall survival and safety. Patients were enrolled from Jan/2019 to Dec/2022. The study accrual was placed on hold during 2020-2021 due to the COVID19 pandemic related institutional resource constraints.
Results: As of the data cutoff date of March 6, 2023, a total of 12 patients were enrolled. The median follow up time was 42.2 months. The median age for the enrolled population was 66 years, female 25%, high-risk cytogenetics 42%, all subjects were IMiD refractory, CD38 refractory 83%. The median lines of prior therapies were 5. Eight patients were dose-limiting toxicity evaluable and dose escalation occurred from the 5mg cohort (0 DLTs out of 3 subjects) and from the 10mg cohort (0 DLTs out of 3 subject). In the 15mg cohort, one DLT occurred out of 2 subjects.
The most common adverse events were anemia (83%), decreased platelet count (50%), dyspnea (50%), and increased creatinine (41.7%). TEAEs by maximum severity grade occurring in at least 25% of subjects are shown in Table 1.
The best response observed in this trial was a VGPR in one subject. The overall response rate was 25%. The median progression-free survival time was 3.2 months, and the overall survival time was 15.8 months.
The study was terminated early due to withdrawal of sponsor funding for not meeting accrual goals during the COVID19 pandemic.
Conclusions: Ruxolitinib may have an acceptable safety profile in combination with carfilzomib at a dose of 10 mg po bid. Despite early encouraging data with 15 mg, the trial could not conclude the safety of this dose. In this proof-of-principle trial, ruxolitinib may have the potential to overcome refractoriness to carfilzomib. However, more studies are needed.
