Cellular and T cell engager Immunotherapy
Poster Session 1
P-051: Safety and efficacy of chimeric antigen receptor T cell therapy in patients with relapse or refractory multiple myeloma and hepatitis B virus-infection
Wednesday, September 27, 2023
1:30 PM - 2:30 PM EEST

Ying Wang, MD
No. 99 West Huaihai Road, Xuzhou 221002, China
Xuzhou Medical University
Xuzhou, Jiangsu, China (People's Republic)
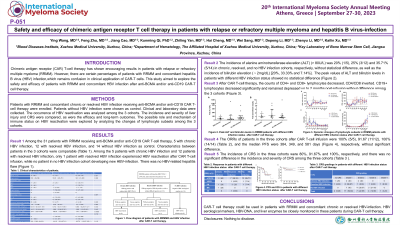
Introduction: Chimeric antigen receptor (CAR) T-cell therapy has shown encouraging results in patients with relapse or refractory multiple myeloma (RRMM). However, there are certain percentages of patients with RRMM and concomitant hepatitis B virus (HBV) infection, which remains confusion in clinical application of CAR-T cells. This study aimed to explore the safety and efficacy of patients with RRMM and concomitant HBV infection after anti-BCMA and/or anti-CD19 CAR-T cell therapy.
Methods: Patients with RRMM and concomitant chronic or resolved HBV infection receiving anti-BCMA and/or anti-CD19 CAR T-cell therapy were enrolled. Patients without HBV infection were choosed as control. Clinical and laboratory datda were collected. The occurrence of HBV reactivation was analyzed among the 3 cohorts. The incidence and severity of liver injury and CRS were compared, as were the efficacy and long-term outcomes. The possible role and mechanism of immune status on HBV reactivation were explored by analyzing the changes of lymphocyte subsets among the 3 cohorts.
Results: Among the 5 patients with chronic HBV infection and 12 patients with resolved HBV infection, only 1 patient with resolved HBV infection experienced HBV reactivation after CAR T-cell infusion, while no patient in no HBV infection cohort developing new HBV-infection. There was no HBV-related hepatitis flare. The incidence of alanine aminotransferase elevation (> 80U/L) was 20% (1/5), 25% (3/12) and 35.71% (5/14) in chronic, resolved, and no HBV infection cohorts, respectively, without statistical difference. After CAR T-cell therapy, the counts of CD4+ and CD8+ lymphocytes decreased, CD4/CD8 inverted. CD19+ lymphocytes decreased significantly and remained depressed up to 2 months post-infusion without difference among the 3 cohorts. The ORRs of patients in the three cohorts after CAR T-cell infusion were 100% (5/5), 91.67 (11/12), 100% (14/14), and the median PFS were 384, 349, and 581 days, respectively, without significant difference. The incidence of CRS in the three cohorts were 80%, 91.67% and 100%, respectively, and there was no significant difference in the incidence and severity of CRS among the three cohorts.
Conclusions: CAR-T cell therapy could be used in patients with RRMM and concomitant chronic or resolved HBV-infection. HBV serological markers, HBV-DNA, and liver enzymes be closely monitored in these patients during CAR-T cell therapy.
Methods: Patients with RRMM and concomitant chronic or resolved HBV infection receiving anti-BCMA and/or anti-CD19 CAR T-cell therapy were enrolled. Patients without HBV infection were choosed as control. Clinical and laboratory datda were collected. The occurrence of HBV reactivation was analyzed among the 3 cohorts. The incidence and severity of liver injury and CRS were compared, as were the efficacy and long-term outcomes. The possible role and mechanism of immune status on HBV reactivation were explored by analyzing the changes of lymphocyte subsets among the 3 cohorts.
Results: Among the 5 patients with chronic HBV infection and 12 patients with resolved HBV infection, only 1 patient with resolved HBV infection experienced HBV reactivation after CAR T-cell infusion, while no patient in no HBV infection cohort developing new HBV-infection. There was no HBV-related hepatitis flare. The incidence of alanine aminotransferase elevation (> 80U/L) was 20% (1/5), 25% (3/12) and 35.71% (5/14) in chronic, resolved, and no HBV infection cohorts, respectively, without statistical difference. After CAR T-cell therapy, the counts of CD4+ and CD8+ lymphocytes decreased, CD4/CD8 inverted. CD19+ lymphocytes decreased significantly and remained depressed up to 2 months post-infusion without difference among the 3 cohorts. The ORRs of patients in the three cohorts after CAR T-cell infusion were 100% (5/5), 91.67 (11/12), 100% (14/14), and the median PFS were 384, 349, and 581 days, respectively, without significant difference. The incidence of CRS in the three cohorts were 80%, 91.67% and 100%, respectively, and there was no significant difference in the incidence and severity of CRS among the three cohorts.
Conclusions: CAR-T cell therapy could be used in patients with RRMM and concomitant chronic or resolved HBV-infection. HBV serological markers, HBV-DNA, and liver enzymes be closely monitored in these patients during CAR-T cell therapy.
