Cellular and T cell engager Immunotherapy
Poster Session 1
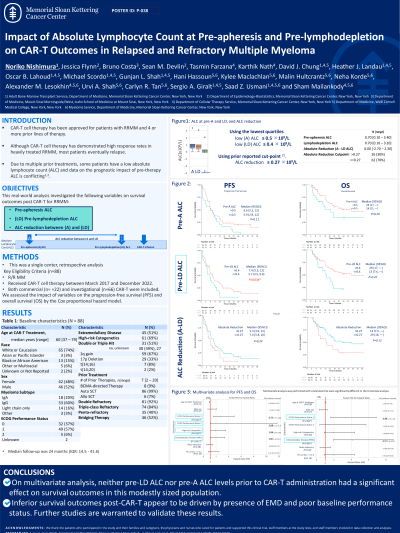
P-038: Impact of Absolute Lymphocyte Count at pre-apheresis and pre-lymphodepletion on Chimeric Antigen Receptor (CAR)-T Therapy Outcomes in Relapsed Refractory Multiple Myeloma (RRMM)
Wednesday, September 27, 2023
1:30 PM - 2:30 PM EEST
Noriko Nishimura, MD, PhD (she/her/hers)
Research Fellow, Medical Oncology Service
Department of Medicine, Memorial Sloan Kettering Cancer Center, United States
Introduction: CAR-T cell therapy has been approved for patients with RRMM and 4 or more prior lines of therapy. Due to multiple prior treatments, some patients have a low absolute lymphocyte count (ALC) and data on the prognostic impact of pre-therapy ALC is conflicting. This real-world analysis investigated pre-apheresis (A) and pre-lymphodepletion (LD) ALC, and the ALC reduction between A and LD, on survival outcomes post CAR-T for RRMM.
Methods: This was a single center, retrospective analysis of 88 patients with RRMM who received CAR-T cell therapy between March 2017 and December 2022. Both commercial (n=22) (BCMA-directed), and investigational (n=66) (BCMA- or GPRC5D-directed) CAR-T were included. We assessed the impact of Pre-A and Pre-LD ALC as well as the reduction in ALC (measured as the difference between pre-LD and pre-A ALC) on the progression-free survival (PFS) and overall survival (OS) using the Cox proportional hazard models.
Results: The median age was 60 years (range, 37–79), of whom 52% were male. The median number of prior lines of therapy was 7 (range: 2–20). Extramedullary disease (EMD) was present in 51%, and 52% of patients received bridging therapy. The median pre-A and pre-LD ALC was 0.7×109/L (range, 0.1–3.4) and 0.7×109/L (range, 0.1–3.1), respectively. The median absolute reduction in ALC was 0.0 (range, -2.7 to 2.3). Using the lowest quartiles, low pre-A ALC and low pre-LD ALC were defined as ≤ 0.5 ×109/L and ≤ 0.4x109/L, respectively. A high reduction was set ≥ 0.27 ×109/L, as described in a prior study. The median follow-up duration post CAR-T infusion was 24 months.
There was no significant difference in PFS with either a low vs. high pre-A ALC (HR 1.52, 95% CI 0.92–2.50, p=0.11), low vs. high pre-LD ALC (HR 1.57, 95%CI 0.93–2.68, p=0.10), or a high absolute reduction in ALC between these timepoints (HR 1.39, 95%CI 0.82–2.36, p=0.24). On multivariate analysis, only EMD, high-risk cytogenetics, and ECOG-score of 1/2 were independently associated with a significantly inferior PFS. Regarding OS, on univariate analysis, low pre-LD ALC was significantly associated with a shorter OS (median OS, 13 vs. 29 months, HR 0.47, 95% CI 0.24–0.92, p=0.032), as was presence of EMD, double refractory status, and Revised-International Staging System (R-ISS) of 2/3. Low pre-A ALC and a high absolute reduction in ALC between A and LD (≥0.27) had no significant impact on OS. On multivariate analysis, only EMD was associated with a significantly shorter OS (HR 4.17, 95% CI 1.96–8.87, p< 0.001).
Conclusions: On multivariate analysis, the pre-A, -pre-LD, and the absolute reduction in ALC prior to CAR-T administration had no significant impact on either PFS or OS. Inferior survival outcomes post-CAR-T appear to be driven by previously recognized factors like the presence of EMD, high-risk cytogenetics, and reduced baseline performance status. Of note, all patients had an ALC > 0.1 X 109/L and the impact of pre-treatment ALC below this level cannot be assessed from this analysis.
Methods: This was a single center, retrospective analysis of 88 patients with RRMM who received CAR-T cell therapy between March 2017 and December 2022. Both commercial (n=22) (BCMA-directed), and investigational (n=66) (BCMA- or GPRC5D-directed) CAR-T were included. We assessed the impact of Pre-A and Pre-LD ALC as well as the reduction in ALC (measured as the difference between pre-LD and pre-A ALC) on the progression-free survival (PFS) and overall survival (OS) using the Cox proportional hazard models.
Results: The median age was 60 years (range, 37–79), of whom 52% were male. The median number of prior lines of therapy was 7 (range: 2–20). Extramedullary disease (EMD) was present in 51%, and 52% of patients received bridging therapy. The median pre-A and pre-LD ALC was 0.7×109/L (range, 0.1–3.4) and 0.7×109/L (range, 0.1–3.1), respectively. The median absolute reduction in ALC was 0.0 (range, -2.7 to 2.3). Using the lowest quartiles, low pre-A ALC and low pre-LD ALC were defined as ≤ 0.5 ×109/L and ≤ 0.4x109/L, respectively. A high reduction was set ≥ 0.27 ×109/L, as described in a prior study. The median follow-up duration post CAR-T infusion was 24 months.
There was no significant difference in PFS with either a low vs. high pre-A ALC (HR 1.52, 95% CI 0.92–2.50, p=0.11), low vs. high pre-LD ALC (HR 1.57, 95%CI 0.93–2.68, p=0.10), or a high absolute reduction in ALC between these timepoints (HR 1.39, 95%CI 0.82–2.36, p=0.24). On multivariate analysis, only EMD, high-risk cytogenetics, and ECOG-score of 1/2 were independently associated with a significantly inferior PFS. Regarding OS, on univariate analysis, low pre-LD ALC was significantly associated with a shorter OS (median OS, 13 vs. 29 months, HR 0.47, 95% CI 0.24–0.92, p=0.032), as was presence of EMD, double refractory status, and Revised-International Staging System (R-ISS) of 2/3. Low pre-A ALC and a high absolute reduction in ALC between A and LD (≥0.27) had no significant impact on OS. On multivariate analysis, only EMD was associated with a significantly shorter OS (HR 4.17, 95% CI 1.96–8.87, p< 0.001).
Conclusions: On multivariate analysis, the pre-A, -pre-LD, and the absolute reduction in ALC prior to CAR-T administration had no significant impact on either PFS or OS. Inferior survival outcomes post-CAR-T appear to be driven by previously recognized factors like the presence of EMD, high-risk cytogenetics, and reduced baseline performance status. Of note, all patients had an ALC > 0.1 X 109/L and the impact of pre-treatment ALC below this level cannot be assessed from this analysis.
