Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-252: Impact of belantamab mafodotin vs pomalidomide/low-dose dexamethasone treatment on health-related quality of life and vision-related functioning in patients with relapsed/refractory multiple myeloma
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST
.jpg)
Meletios A. Dimopoulos, MD
Professor and Chairman of the Department of Clinical Therapeutics
National and Kapodistrian University of Athens, United States
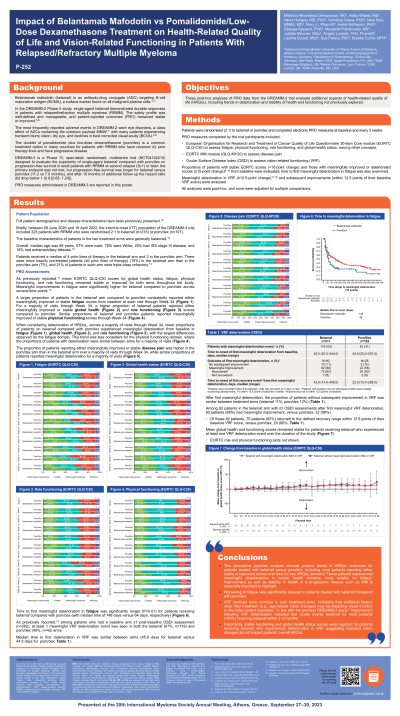
Introduction: The Phase 3, open-label, randomised, DREAMM-3 trial (NCT04162210) assessed single-agent belantamab mafodotin (belamaf), an antibody-drug conjugate targeting BCMA, vs pomalidomide + low-dose dexamethasone (Pd) in adults with relapsed/refractory multiple myeloma (RRMM) at second relapse or later. Trends in health-related quality of life (HRQL) and vision-related functioning (VRF) in DREAMM-3 are reported.
Methods: Patients (pts) were randomised (2:1) to belamaf or Pd and completed electronic pt-reported outcome measures including EORTC QLQ-C30 (fatigue, physical and role functioning, global health), EORTC MM module (QLQ-MY20, disease pain), and the Ocular Surface Disease Index (OSDI, impact of ocular adverse events of special interest on VRF) at baseline (BL) and every 3 weeks. Proportions of pts with meaningful deterioration from BL in EORTC scores (≥10-point change) and time to first meaningful deterioration in fatigue were assessed. Meaningful deterioration in VRF (≥12.5-point change) and subsequent improvements were analysed. All were post hoc analyses.
Results: 325 patients with RRMM were enrolled (belamaf, n=218; Pd, n=107). Compared to Pd, lower proportions of pts on belamaf experienced meaningful deterioration from BL in fatigue, functioning (physical, role), and global health; this pattern was seen across most visits through Week 31 and was most notable and consistent for role functioning and fatigue. For worsening disease pain, no difference was noted between arms. Time to first meaningful deterioration in fatigue was significantly delayed (P < 0.01) for pts receiving belamaf compared with Pd (median 148 days vs 64). Among pts with BL and ≥1 post-BL OSDI assessment (n=262), meaningful VRF deterioration was seen in both belamaf (67%) and Pd (49%) arms. Median days to first meaningful VRF deterioration was 45 for belamaf vs 44.5 in Pd. Lack of improvement after meaningful deterioration was similar across arms (belamaf 11%, Pd 12%). Among 92 pts in the belamaf arm with ≥3 OSDI assessments after first meaningful VRF deterioration, 82 (89%) pts had meaningful improvement, including 75 who returned to within 12.5 points of BL VRF score (defined recovery range). Mean global health and functioning scores remained stable for pts receiving belamaf who experienced VRF deterioration over the study.
Conclusions: This descriptive analysis suggests positive trends in HRQL outcomes for pts treated with belamaf vs Pd, including fewer pts experiencing meaningful HRQL deterioration related to this progressive disease, and significantly delayed worsening of fatigue in pts on belamaf. In line with previous studies (DREAMM-2 and -3), improvement following VRF deterioration showed that ocular issues resolved for most pts receiving belamaf within 3 months. Importantly, stable functioning scores and global health status were seen for pts receiving belamaf who experienced deterioration in VRF, suggesting vision changes did not impact pts’ overall HRQL.
Methods: Patients (pts) were randomised (2:1) to belamaf or Pd and completed electronic pt-reported outcome measures including EORTC QLQ-C30 (fatigue, physical and role functioning, global health), EORTC MM module (QLQ-MY20, disease pain), and the Ocular Surface Disease Index (OSDI, impact of ocular adverse events of special interest on VRF) at baseline (BL) and every 3 weeks. Proportions of pts with meaningful deterioration from BL in EORTC scores (≥10-point change) and time to first meaningful deterioration in fatigue were assessed. Meaningful deterioration in VRF (≥12.5-point change) and subsequent improvements were analysed. All were post hoc analyses.
Results: 325 patients with RRMM were enrolled (belamaf, n=218; Pd, n=107). Compared to Pd, lower proportions of pts on belamaf experienced meaningful deterioration from BL in fatigue, functioning (physical, role), and global health; this pattern was seen across most visits through Week 31 and was most notable and consistent for role functioning and fatigue. For worsening disease pain, no difference was noted between arms. Time to first meaningful deterioration in fatigue was significantly delayed (P < 0.01) for pts receiving belamaf compared with Pd (median 148 days vs 64). Among pts with BL and ≥1 post-BL OSDI assessment (n=262), meaningful VRF deterioration was seen in both belamaf (67%) and Pd (49%) arms. Median days to first meaningful VRF deterioration was 45 for belamaf vs 44.5 in Pd. Lack of improvement after meaningful deterioration was similar across arms (belamaf 11%, Pd 12%). Among 92 pts in the belamaf arm with ≥3 OSDI assessments after first meaningful VRF deterioration, 82 (89%) pts had meaningful improvement, including 75 who returned to within 12.5 points of BL VRF score (defined recovery range). Mean global health and functioning scores remained stable for pts receiving belamaf who experienced VRF deterioration over the study.
Conclusions: This descriptive analysis suggests positive trends in HRQL outcomes for pts treated with belamaf vs Pd, including fewer pts experiencing meaningful HRQL deterioration related to this progressive disease, and significantly delayed worsening of fatigue in pts on belamaf. In line with previous studies (DREAMM-2 and -3), improvement following VRF deterioration showed that ocular issues resolved for most pts receiving belamaf within 3 months. Importantly, stable functioning scores and global health status were seen for pts receiving belamaf who experienced deterioration in VRF, suggesting vision changes did not impact pts’ overall HRQL.
