Other plasma cell disorders
Poster Session 3
P-422: Impact of early response and CXCR4 mutation status on progression-free survival with ibrutinib-based therapy in Waldenström macroglobulinemia: A post hoc analysis of the iNNOVATE trial
Friday, September 29, 2023
1:15 PM - 2:15 PM EEST

Jorge J. Castillo, MD (he/him/his)
Associate Professor of Medicine
Dana-Farber Cancer Institute
Boston, Massachusetts, United States
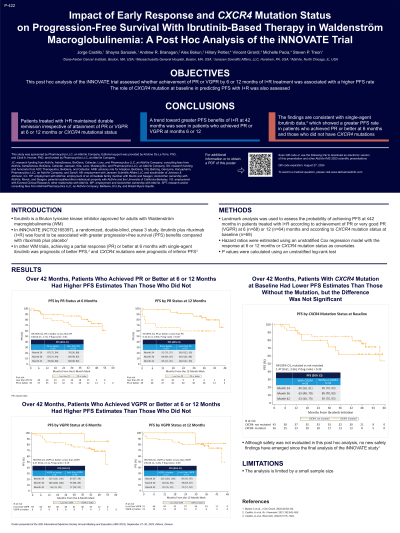
Introduction: Ibrutinib is a Bruton tyrosine kinase inhibitor approved for adults with Waldenström macroglobulinemia (WM). In iNNOVATE (NCT02165397), a randomized, double-blind, phase 3 study, ibrutinib plus rituximab (I+R) was associated with greater progression-free survival (PFS) benefits compared with rituximab plus placebo (Buske C et al. J Clin Oncol. 2021). In patients with WM, achieving a partial response (PR) or better at 6 months with single-agent ibrutinib was prognostic of better PFS (Castillo JJ et al. Br J Haematol. 2021), and CXCR4 mutations were prognostic of inferior PFS (Castillo JJ et al. Blood Adv. 2022). This post hoc analysis of iNNOVATE assessed whether achievement of PR or very good PR (VGPR) by month 6 or 12 of I+R treatment was associated with a higher PFS rate. The role of CXCR4 mutation at baseline in predicting PFS with I+R was also assessed.
Methods: We used landmark analysis to assess the probability of achieving PFS at ≤42 months in patients treated with I+R according to achievement of PR or VGPR at 6 (n=68) or 12 (n=64) months and according to CXCR4 mutation status at baseline (n=69). Hazard ratios were estimated using an unstratified Cox regression model with the response at 6 or 12 months or CXCR4 mutation status as covariates. P values were calculated using an unstratified log-rank test.
Results: Patients who achieved PR or better at 6 months (n=39) had a higher PFS rate at 42 months than patients who did not (n=29) (78% [95% CI 60-88%] vs 68% [95% CI 48-82%]), but the difference over the entire study period was not significant (P=0.41). The difference was significant over the study period between patients who did (n=49) and did not achieve PR (n=15) at 12 months (P=0.027), with 42-month PFS rates of 80% (95% CI 63-90%) and 60% (95% CI 32-80%), respectively. For patients who achieved VGPR or better at 6 months (n=9) versus those who did not (n=59), the 42-month PFS rates were 86% (95% CI 33-98%) versus 72% (95% CI 58-82%), with overall P=0.19. The corresponding values for patients with (n=13) and without VGPR (n=51) at 12 months were 82% (95% CI 45-95%) and 74% (95% CI 57-85%); overall P=0.36. For patients with CXCR4 mutation at baseline (n=26) versus those without mutation (n=43), the PFS rates at 42 months were 63% (95% CI 40-79%) versus 85% (95% CI 70-93%), respectively (overall P=0.39).
Conclusions: Patients treated with I+R maintained durable remission irrespective of CXCR4 mutational status or attainment of PR or VGPR at 6 or 12 months. A trend towards greater PFS benefits of I+R at 42 months was seen in patients who achieved PR or VGPR at months 6 or 12 and those without CXCR4 mutations. The findings are consistent with single-agent ibrutinib data (Castillo JJ et al. Br J Haematol. 2021), which showed a greater PFS rate in patients who achieved PR or better at 6 months and those who did not have CXCR4 mutations. The analysis is limited by a small sample size.
The iNNOVATE study was funded by Pharmacyclics, LLC, an AbbVie company.
Methods: We used landmark analysis to assess the probability of achieving PFS at ≤42 months in patients treated with I+R according to achievement of PR or VGPR at 6 (n=68) or 12 (n=64) months and according to CXCR4 mutation status at baseline (n=69). Hazard ratios were estimated using an unstratified Cox regression model with the response at 6 or 12 months or CXCR4 mutation status as covariates. P values were calculated using an unstratified log-rank test.
Results: Patients who achieved PR or better at 6 months (n=39) had a higher PFS rate at 42 months than patients who did not (n=29) (78% [95% CI 60-88%] vs 68% [95% CI 48-82%]), but the difference over the entire study period was not significant (P=0.41). The difference was significant over the study period between patients who did (n=49) and did not achieve PR (n=15) at 12 months (P=0.027), with 42-month PFS rates of 80% (95% CI 63-90%) and 60% (95% CI 32-80%), respectively. For patients who achieved VGPR or better at 6 months (n=9) versus those who did not (n=59), the 42-month PFS rates were 86% (95% CI 33-98%) versus 72% (95% CI 58-82%), with overall P=0.19. The corresponding values for patients with (n=13) and without VGPR (n=51) at 12 months were 82% (95% CI 45-95%) and 74% (95% CI 57-85%); overall P=0.36. For patients with CXCR4 mutation at baseline (n=26) versus those without mutation (n=43), the PFS rates at 42 months were 63% (95% CI 40-79%) versus 85% (95% CI 70-93%), respectively (overall P=0.39).
Conclusions: Patients treated with I+R maintained durable remission irrespective of CXCR4 mutational status or attainment of PR or VGPR at 6 or 12 months. A trend towards greater PFS benefits of I+R at 42 months was seen in patients who achieved PR or VGPR at months 6 or 12 and those without CXCR4 mutations. The findings are consistent with single-agent ibrutinib data (Castillo JJ et al. Br J Haematol. 2021), which showed a greater PFS rate in patients who achieved PR or better at 6 months and those who did not have CXCR4 mutations. The analysis is limited by a small sample size.
The iNNOVATE study was funded by Pharmacyclics, LLC, an AbbVie company.
