Treatment of Newly Diagnosed Myeloma - Transplant Eligible
Poster Session 1
P-161: IMPACT OF INDUCTION TREATMENT ON THE SURVIVAL OF PATIENTS WITH MULTIPLE MYELOMA CANDIDATES FOR AUTOLOGOUS STEM CELL TRANSPLANTATION. EXPERIENCE OF A CENTER.
Wednesday, September 27, 2023
1:30 PM - 2:30 PM EEST

Raquel Santoja
Hematologist
Hospital Universitari Arnau de Vilanova, Lleida
LLEIDA, Catalonia, Spain
Introduction: Actually, despite the incorporation of new treatments in multiple myeloma, autologous hematopoietic stem cell transplantation (ASCT) continues to be the frontline treatment for those patients who are candidates to intensive treatment.
Methods: A retrospective analysis was performed in multiple myeloma patients who received ASCT from 1995 to 2020. The objective of our study was to analyze the evolution of progression-free survival (PFS) and overall survival (OS) in patients with multiple myeloma undergoing ASCT at our center. We have analyzed the results based on the type of induction received according to current clinical practice: chemotherapy (CT), Bortezomib-Dexamethasone (VD) or triplet therapy with Bortezomib, Thalidomide and Dexamethasone (VTD). We analyzed the impact of maintenance treatment with Lenalidomide in patients who have received VTD therapy. Inductions treatments were performed in different periods of time: QT (1995-2011), VD (2011-2014) and VTD (2015-2020).
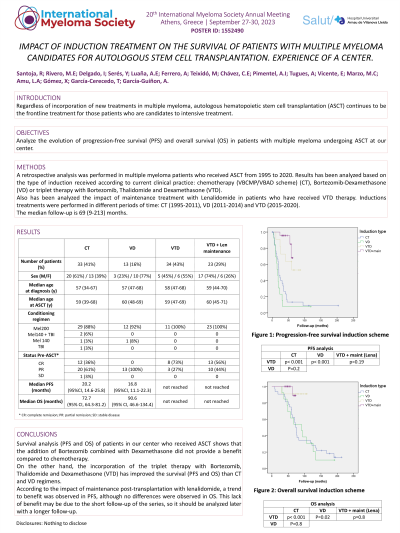
Results: Eighty patients have been included, 52 (65%) of them were male. The median age at diagnosis was 58 (34-70) years and at ASCT was 59 (39-71) years. The induction treatment received in 33 (41%) patients was CT based on VBMCP/VBAD regimen, 13 (16%) patients with VD and 34 (43%) patients with VTD. Twenty-three (29%) patients with VTD schedule received maintenance therapy with lenalidomide.
Median PFS was 20.2 (95%CI, 14.6-25.8) months in patients who received CT and 16.8 (95%CI, 11.1-22.3) months for VD. Median PFS has not been reached in patients who received VTD (figure 1). PFS analysis showed statistically significant differences between VTD and QT (p < 0.001) and VD (p < 0.001). No significant differences was observed between QT and VD groups (p=0.2). Patients who received maintenance show a higher PFS than those who did not, despite difference is not statistically significant (p=0.19). Median overall survival (OS) was similar in patients who received CT and VD: 72.7 (95% CI, 64.3-81.2) months and 90.6 (46.6-134.4) months, respectively. Median OS was not reached in patients who received VTD. The OS analysis showed statistically significant difference between VTD and QT (p < 0.001) and VD (p=0.002). No differences were observed in overall survival (p=0.8) in patients who received maintenance with lenalidomide (figure 2).
Conclusions: Survival analysis (PFS and OS) of patients in our center who received ASCT shows that the addition of Bortezomib combined with Dexamethasone did not provide a benefit compared to polychemotherapy. On the other hand, the incorporation of the triplet therapy with Bortezomib, Thalidomide and Dexamethasone (VTD) has improved the survival (PFS and OS) than CT and VD regimens. According to the impact of maintenance post-transplantation with lenalidomide, a trend to benefit was observed in PFS, although no differences were observed in OS. This lack of benefit may be due to the short follow-up of the series, so it should be analyzed later with a longer follow-up.
Methods: A retrospective analysis was performed in multiple myeloma patients who received ASCT from 1995 to 2020. The objective of our study was to analyze the evolution of progression-free survival (PFS) and overall survival (OS) in patients with multiple myeloma undergoing ASCT at our center. We have analyzed the results based on the type of induction received according to current clinical practice: chemotherapy (CT), Bortezomib-Dexamethasone (VD) or triplet therapy with Bortezomib, Thalidomide and Dexamethasone (VTD). We analyzed the impact of maintenance treatment with Lenalidomide in patients who have received VTD therapy. Inductions treatments were performed in different periods of time: QT (1995-2011), VD (2011-2014) and VTD (2015-2020).
Results: Eighty patients have been included, 52 (65%) of them were male. The median age at diagnosis was 58 (34-70) years and at ASCT was 59 (39-71) years. The induction treatment received in 33 (41%) patients was CT based on VBMCP/VBAD regimen, 13 (16%) patients with VD and 34 (43%) patients with VTD. Twenty-three (29%) patients with VTD schedule received maintenance therapy with lenalidomide.
Median PFS was 20.2 (95%CI, 14.6-25.8) months in patients who received CT and 16.8 (95%CI, 11.1-22.3) months for VD. Median PFS has not been reached in patients who received VTD (figure 1). PFS analysis showed statistically significant differences between VTD and QT (p < 0.001) and VD (p < 0.001). No significant differences was observed between QT and VD groups (p=0.2). Patients who received maintenance show a higher PFS than those who did not, despite difference is not statistically significant (p=0.19). Median overall survival (OS) was similar in patients who received CT and VD: 72.7 (95% CI, 64.3-81.2) months and 90.6 (46.6-134.4) months, respectively. Median OS was not reached in patients who received VTD. The OS analysis showed statistically significant difference between VTD and QT (p < 0.001) and VD (p=0.002). No differences were observed in overall survival (p=0.8) in patients who received maintenance with lenalidomide (figure 2).
Conclusions: Survival analysis (PFS and OS) of patients in our center who received ASCT shows that the addition of Bortezomib combined with Dexamethasone did not provide a benefit compared to polychemotherapy. On the other hand, the incorporation of the triplet therapy with Bortezomib, Thalidomide and Dexamethasone (VTD) has improved the survival (PFS and OS) than CT and VD regimens. According to the impact of maintenance post-transplantation with lenalidomide, a trend to benefit was observed in PFS, although no differences were observed in OS. This lack of benefit may be due to the short follow-up of the series, so it should be analyzed later with a longer follow-up.
