MRD Assessment and role in Myeloma
Poster Session 1
P-079: Impact of treatment effect on measurable residual disease (MRD) and progression-free survival (PFS): an aggregate data analysis from randomized clinical trials in multiple myeloma (MM)
Wednesday, September 27, 2023
1:30 PM - 2:30 PM EEST
.jpg)
Bruno Paiva, PhD
Director Flow Cytometry Core
Clínica Universidad de Navarra (CUN), Centro de Investigación Médica Aplicada (CIMA LAB Diagnostics), IDISNA, CIBERONC
Pamplona, Navarra, Spain
Introduction: Novel regimens are needed to increase cure rates in MM, but new studies will not have a (positive or negative) readout for many years due to the unprecedented PFS and overall survival achieved with current therapies. Assessment of MRD is one of the most relevant prognostic factors and outperforms conventional methods of response assessment in MM. However, the role of MRD as a surrogate of treatment efficacy for potential use as an endpoint in clinical trials, remains uncertain.
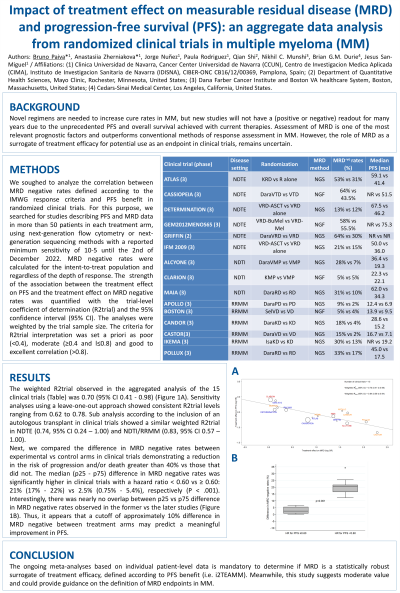
Methods: We soughed to analyze the correlation between MRD negative rates defined according to the IMWG response criteria and PFS benefit in randomized clinical trials. For this purpose, we searched for studies describing PFS and MRD data in more than 50 patients in each treatment arm, using next-generation flow cytometry or next-generation sequencing methods with a reported minimum sensitivity of 10-5 until the 2nd of December 2022. MRD negative rates were calculated for the intent-to-treat population and regardless of the depth of response.
The strength of the association between the treatment effect on PFS and the treatment effect on MRD negative rates was quantified with the trial-level coefficient of determination (R2trial) and the 95% confidence interval (95% CI). The analyses were weighted by the trial sample size. The criteria for R2trial interpretation was set a priori as poor ( < 0.4), moderate (≥0.4 and l≤0.8) and good to excellent correlation (>0.8).
Results: The weighted R2trial observed in the aggregated analysis of the 15 clinical trials was 0.70 (95% CI 0.41 - 0.98). Sensitivity analyses using a leave-one-out approach showed consistent R2trial levels ranging from 0.62 to 0.78. Sub analysis according to the inclusion of an autologous transplant in clinical trials showed a similar weighted R2trial in NDTE (0.74, 95% CI 0.24 – 1.00) and NDTI/RRMM (0.83, 95% CI 0.57 – 1.00).
Next, we compared the difference in MRD negative rates between experimental vs control arms in clinical trials demonstrating a reduction in the risk of progression and/or death greater than 40% vs those that did not. The median (p25 - p75) difference in MRD negative rates was significantly higher in clinical trials with a hazard ratio < 0.60 vs ≥ 0.60: 21% (17% - 22%) vs 2.5% (0.75% - 5.4%), respectively (P < .001). Interestingly, there was nearly no overlap between p25 vs p75 difference in MRD negative rates observed in the former vs the later studies. Thus, it appears that a cutoff of approximately 10% difference in MRD negative rates between treatment arms may predict a meaningful improvement in PFS.
Conclusions: The ongoing meta-analyses based on individual patient-level data is mandatory to determine if MRD is a statistically robust surrogate of treatment efficacy, defined according to PFS benefit (i.e. i2TEAMM). Meanwhile, this study suggests moderate value and could provide guidance on the definition of MRD endpoints in MM.
Methods: We soughed to analyze the correlation between MRD negative rates defined according to the IMWG response criteria and PFS benefit in randomized clinical trials. For this purpose, we searched for studies describing PFS and MRD data in more than 50 patients in each treatment arm, using next-generation flow cytometry or next-generation sequencing methods with a reported minimum sensitivity of 10-5 until the 2nd of December 2022. MRD negative rates were calculated for the intent-to-treat population and regardless of the depth of response.
The strength of the association between the treatment effect on PFS and the treatment effect on MRD negative rates was quantified with the trial-level coefficient of determination (R2trial) and the 95% confidence interval (95% CI). The analyses were weighted by the trial sample size. The criteria for R2trial interpretation was set a priori as poor ( < 0.4), moderate (≥0.4 and l≤0.8) and good to excellent correlation (>0.8).
Results: The weighted R2trial observed in the aggregated analysis of the 15 clinical trials was 0.70 (95% CI 0.41 - 0.98). Sensitivity analyses using a leave-one-out approach showed consistent R2trial levels ranging from 0.62 to 0.78. Sub analysis according to the inclusion of an autologous transplant in clinical trials showed a similar weighted R2trial in NDTE (0.74, 95% CI 0.24 – 1.00) and NDTI/RRMM (0.83, 95% CI 0.57 – 1.00).
Next, we compared the difference in MRD negative rates between experimental vs control arms in clinical trials demonstrating a reduction in the risk of progression and/or death greater than 40% vs those that did not. The median (p25 - p75) difference in MRD negative rates was significantly higher in clinical trials with a hazard ratio < 0.60 vs ≥ 0.60: 21% (17% - 22%) vs 2.5% (0.75% - 5.4%), respectively (P < .001). Interestingly, there was nearly no overlap between p25 vs p75 difference in MRD negative rates observed in the former vs the later studies. Thus, it appears that a cutoff of approximately 10% difference in MRD negative rates between treatment arms may predict a meaningful improvement in PFS.
Conclusions: The ongoing meta-analyses based on individual patient-level data is mandatory to determine if MRD is a statistically robust surrogate of treatment efficacy, defined according to PFS benefit (i.e. i2TEAMM). Meanwhile, this study suggests moderate value and could provide guidance on the definition of MRD endpoints in MM.
