Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-302: ANCHOR (OP-104): MELFLUFEN PLUS DEXAMETHASONE AND DARATUMUMAB OR BORTEZOMIB IN RELAPSED/REFRACTORY MULTIPLE MYELOMA (RRMM)—FINAL EFFICACY AND SAFETY RESULTS
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST

Enrique M. Ocio, MD, PhD
Head of the Hematology Department
Hospital Universitario Marqués de Valdecilla (IDIVAL), Santander, Spain
Santander, Cantabria, Spain
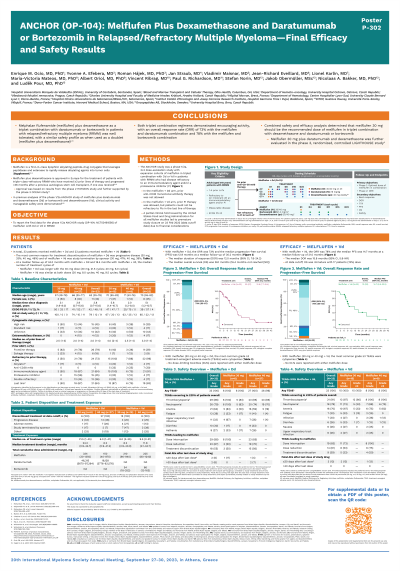
Introduction: Melphalan flufenamide (melflufen), a first-in-class peptide-drug conjugate (PDC), plus dexamethasone (dex) is approved for use in Europe in patients (pts) with triple-class refractory RRMM who have received ≥3 prior lines of therapy (LoTs) and progressed >36 mo after a prior autologous stem cell transplant if received. Here, we report the final data for the phase 1/2a ANCHOR study of melflufen with bortezomib + dex (Vd) or daratumumab + dex (Dd) (NCT03481556).
Methods: Pts had RRMM refractory/intolerant to an IMiD and/or a proteasome inhibitor (PI) and 1-4 prior LoTs. Vd arm: PI in prior LoT (but not refractoriness in the last LoT) was allowed. Dd arm: prior anti-CD38 monoclonal antibody therapy prohibited. All pts received intravenous (IV) melflufen (30 or 40 mg, day 1 per cycle). Vd arm: bortezomib 1.3 mg/m2 subcutaneous, days 1, 4, 8, and 11 + oral dex (20 mg on days 1, 4, 8, and 11 and 40 mg on days 15 and 22; dose reduced if aged ≥75 y). Dd arm: daratumumab 16 mg/kg IV once per wk (2 cycles), every 2 wk (4 cycles), then every 4 wk + oral dex (40 mg on days 1, 8, 15, and 22). Primary objectives: determine the optimal melflufen dose in each combination (phase 1); assess overall response rate (ORR; phase 2).
Results: As of 9 Feb 2022 (data cutoff date), 23 pts received melflufen (30 mg, n=15; 40 mg, n=8) +Vd and 33 melflufen (30 mg, n=6; 40 mg, n=27) +Dd. The partial clinical hold issued by the US Food and Drug Administration led to premature study termination on 23 Feb 2022.
Vd arm: Median (range) treatment duration was 8.3 mo (2.8-40.0) in the 30-mg cohort and 12.0 mo (2.1-34.7) in the 40-mg cohort. ORR for the pooled cohorts was 78% (2 complete response or better [≥CR], 5 very good partial response [VGPR], 11 partial response [PR]). At a median follow-up of 21 mo, the median progression-free survival (PFS) was 14.7 mo (95% CI, 8.5-33.5); overall survival (OS) was immature with 17 pts (74%) alive at data cutoff. Grade ≥3 treatment-emergent adverse events (TEAEs) were most commonly cytopenias and infrequently nonhematologic; thrombocytopenia led to treatment discontinuation in 3 pts. No dose-limiting toxicities (DLTs) and 3 fatal AEs (1 cardiac failure chronic, 2 COVID-19 pneumonia) occurred.
Dd arm: Median (range) treatment duration was 24.1 mo (0.9-44.6) in the 30-mg cohort and 6.2 mo (0.9-41.2) in the 40-mg cohort. ORR was 73% (3 ≥CR, 8 VGPR, 13 PR). Median (95% CI) PFS was 12.9 mo (7.7-15.4) and OS was 26.1 mo (16.4-not estimable), at a median follow-up of 30.0 and 32.8 mo, respectively. Thrombocytopenia and neutropenia were the most common grade ≥3 TEAEs and TEAEs leading to treatment discontinuation. Grade ≥3 nonhematologic TEAEs were infrequent. No DLTs and 4 fatal AEs (2 sepsis, 1 cardiac failure chronic, 1 general physical health deterioration) occurred.
Conclusions: Melflufen + Vd or Dd showed encouraging activity in RRMM with 1-4 prior LoTs. Safety and efficacy analyses determined melflufen 30 mg to be the recommended dose in triplet regimens.
Methods: Pts had RRMM refractory/intolerant to an IMiD and/or a proteasome inhibitor (PI) and 1-4 prior LoTs. Vd arm: PI in prior LoT (but not refractoriness in the last LoT) was allowed. Dd arm: prior anti-CD38 monoclonal antibody therapy prohibited. All pts received intravenous (IV) melflufen (30 or 40 mg, day 1 per cycle). Vd arm: bortezomib 1.3 mg/m2 subcutaneous, days 1, 4, 8, and 11 + oral dex (20 mg on days 1, 4, 8, and 11 and 40 mg on days 15 and 22; dose reduced if aged ≥75 y). Dd arm: daratumumab 16 mg/kg IV once per wk (2 cycles), every 2 wk (4 cycles), then every 4 wk + oral dex (40 mg on days 1, 8, 15, and 22). Primary objectives: determine the optimal melflufen dose in each combination (phase 1); assess overall response rate (ORR; phase 2).
Results: As of 9 Feb 2022 (data cutoff date), 23 pts received melflufen (30 mg, n=15; 40 mg, n=8) +Vd and 33 melflufen (30 mg, n=6; 40 mg, n=27) +Dd. The partial clinical hold issued by the US Food and Drug Administration led to premature study termination on 23 Feb 2022.
Vd arm: Median (range) treatment duration was 8.3 mo (2.8-40.0) in the 30-mg cohort and 12.0 mo (2.1-34.7) in the 40-mg cohort. ORR for the pooled cohorts was 78% (2 complete response or better [≥CR], 5 very good partial response [VGPR], 11 partial response [PR]). At a median follow-up of 21 mo, the median progression-free survival (PFS) was 14.7 mo (95% CI, 8.5-33.5); overall survival (OS) was immature with 17 pts (74%) alive at data cutoff. Grade ≥3 treatment-emergent adverse events (TEAEs) were most commonly cytopenias and infrequently nonhematologic; thrombocytopenia led to treatment discontinuation in 3 pts. No dose-limiting toxicities (DLTs) and 3 fatal AEs (1 cardiac failure chronic, 2 COVID-19 pneumonia) occurred.
Dd arm: Median (range) treatment duration was 24.1 mo (0.9-44.6) in the 30-mg cohort and 6.2 mo (0.9-41.2) in the 40-mg cohort. ORR was 73% (3 ≥CR, 8 VGPR, 13 PR). Median (95% CI) PFS was 12.9 mo (7.7-15.4) and OS was 26.1 mo (16.4-not estimable), at a median follow-up of 30.0 and 32.8 mo, respectively. Thrombocytopenia and neutropenia were the most common grade ≥3 TEAEs and TEAEs leading to treatment discontinuation. Grade ≥3 nonhematologic TEAEs were infrequent. No DLTs and 4 fatal AEs (2 sepsis, 1 cardiac failure chronic, 1 general physical health deterioration) occurred.
Conclusions: Melflufen + Vd or Dd showed encouraging activity in RRMM with 1-4 prior LoTs. Safety and efficacy analyses determined melflufen 30 mg to be the recommended dose in triplet regimens.
